Article Contents
| Korean J Pediatr > Volume 58(2); 2015 |
|
Abstract
Purpose
The purpose of this study was to investigate the importance of initial screening tests for depression and anxiety disorders in children with headache. In addition, this study evaluated whether the Children's Depression Inventory (CDI) and Revised Children's Manifest Anxiety Scale (RCMAS) are suitable for screening symptoms of depression and anxiety.
Methods
A retrospective chart review was conducted of 720 children aged 7-17 years who had visited a pediatric neurology clinic for headaches and were referred to a pediatric psychiatric clinic for psychiatric symptoms from January 2010 to December 2011. All patients completed the CDI and RCMAS. Among them, charts of patients with clinically significant total scores (cutoff>15) for psychiatric symptoms, as defined by the CDI and RCMAS scoring scales, were reviewed.
Results
Nineteen patients had headaches and clinically significant total scores for psychiatric symptoms. The mean age at headache diagnosis was 11.7 years, and 57% were male. Mean duration of headache was 11.5 months. Two point eight percent of the patients were diagnosed with psychiatric disorders including major depression (1.7%), generalized anxiety disorder (1.1%), and bipolar disorder (0.1%). Four patients (0.6%) were diagnosed with attention deficit/hyperactivity disorder (ADHD). Total mean CDI and RCMAS scores of patients referred to the psychiatric clinic were 18.8 and 22.2, respectively. There was no correlation between CDI or RCMAS total scores and headache frequency, duration, or severity.
Headache is common among children and adolescents. Epidemiological studies suggest that 10%-30% of children and adolescents reported weekly or daily headaches and 9%-33% of patients suffer from a primary headache at least monthly1,2,3). Psychiatric comorbidity, especially depression and anxiety, has been well documented in patients with primary headaches. In addition, headache in childhood and adolescence is associated with behavioral and emotional disorders. Psychiatric problems in headache patients are associated with decreased quality of life, poorer prognosis, chronification of disease, and poorer response to treatment4). The early identification of psychiatric problems in patients with headache is crucial also for headache treatment and prognosis. These prevalence and impact, several recent studies suggest that patients with headaches in primary care should receive at least brief screenings for psychiatric disorders4,5). However, in children, the research on the relationship between headache and psychiatric disorders has received less attention.
In our clinical experience, headache patients with psychiatric symptoms had improvement in headache with psychiatric medication and psychotherapy for psychiatric symptoms. The aim of this study was to investigate the importance of initial screening for psychiatric symptoms, especially depression and anxiety, in children with headache.
This study is a retrospective chart review of children, who were seen in a pediatric neurology clinic for headaches and were referred to pediatric psychology clinic for presumed psychiatric disorders from January 2010 to December 2011. A total of 720 patients were sent for headaches diagnoses in a pediatric neurology clinic and 20 of these patients were referred for assessment of psychiatric disorders. This study reviewed the charts of all patients after informed written consent was obtained from each patient's parents.
All patients completed a structured headache questionnaire, which included questions about demographic characteristics and clinical features, and Children's Depression Inventory (CDI) and Revised Manifest Anxiety Scale for Children (RCMAS) at their initial visit to the neurology clinic. Demographic characteristics included age, sex and clinical data about the headache such as first onset age, duration, frequency, nature, locus, presymptoms, headache intensity, associated symptoms, family history of headaches, family history of psychiatric disorders, and medication history including headache or psychiatric medication in the past. A thorough headache history and neurologic examination were also performed by a neurologist.
Headache frequency was the average monthly headache frequency during the last three months. Headache intensity was assessed on an 11-point pain scale (0-10) with 0 indicating 'no headache pain' and 10 indicating 'most severe pain possible'. 1-3 was defined as 'mild'; 4-6 as 'moderate'; and 7-10 as 'severe'. Headache type was classified using the International Classification of Headache Disorders, 2nd edition diagnostic criteria.
Symptoms of depression were measured using the CDI. This is a well-established self-rating screening tool (reliability, 0.87) with 27 statements on rated on a 3-point (0-2) scale. For each statement, the child is asked to select the response that best describes his or her feelings in the preceding two weeks. There is a total CDI score, and 5 subscales: negative mood, interpersonal problem, ineffectiveness, anhedonia, and negative self-esteem. CDI has been validated in children aged 7-17 years and is one of the most commonly used screening methods for childhood depression.
Symptoms of anxiety were measured using the RCMAS. It is a self-reported screening tool (reliability, 0.94) to measure anxiety in children aged 6-19 years. The RCMAS consists of 37 items, each of which requires a yes or no answer. There is a total score, and 3 anxiety subscales: physiological anxiety, worry/oversensitivity, and social concerns. A total scores >15 is considered clinically significant, and children with clinically significant total scores were referred to a pediatric psychiatric clinic for further assessment.
All data were analyzed using the SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Variables data were expressed as mean±standard deviation. Correlation between the mean CDI or RCMAS scores, and headache frequency, duration, and intensity was expressed by the Spearman rank correlation coefficient. A P value of <0.05 was considered statistically significant.
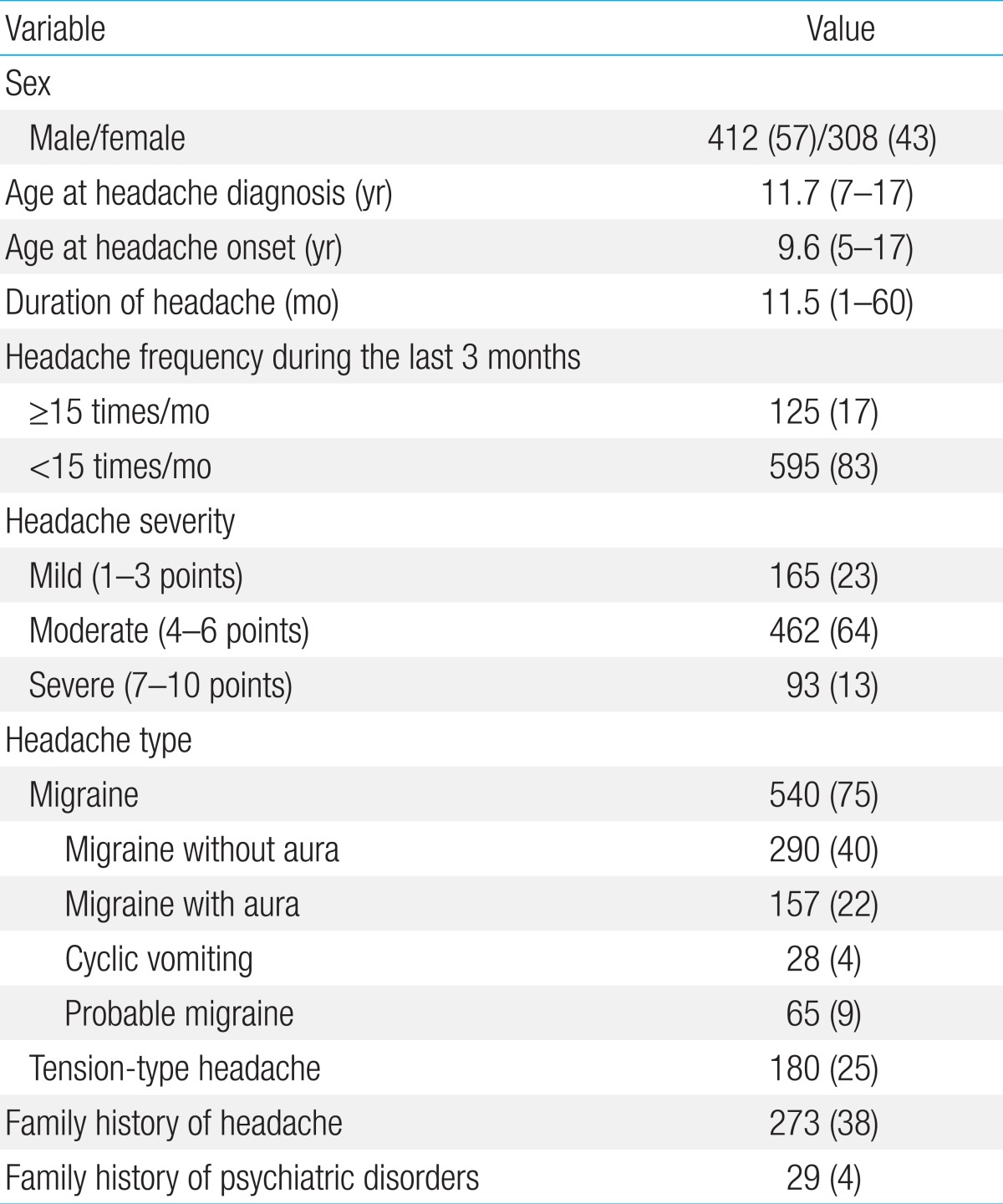
Of the 720 patients, 412 (57%) were males and 308 (43%) were females, with a mean age of 11.7 years (range, 7-17 years). The mean age at onset of headache was 9.6 years (range, 5-17 years). The mean duration of headache was 11.5 months (range, 1-60 months). The headache frequency during the last 3 months were 125 patients (17%) with >15 day/mo, 87 patients (12%) with daily headache.
Five hundred and forty patients (75%) had migraine and 180 patients (25%) had tension-type headache. Two hundred and seventy-three patients (25%) had a family history of migraine and 29 patients (4%) had a family history of depression.
Demographic and clinical characteristics of patients are summarized in Table 1. Twenty patients of 720 headache patients were referred to a pediatric psychology clinic for presumed psychiatric disorders.
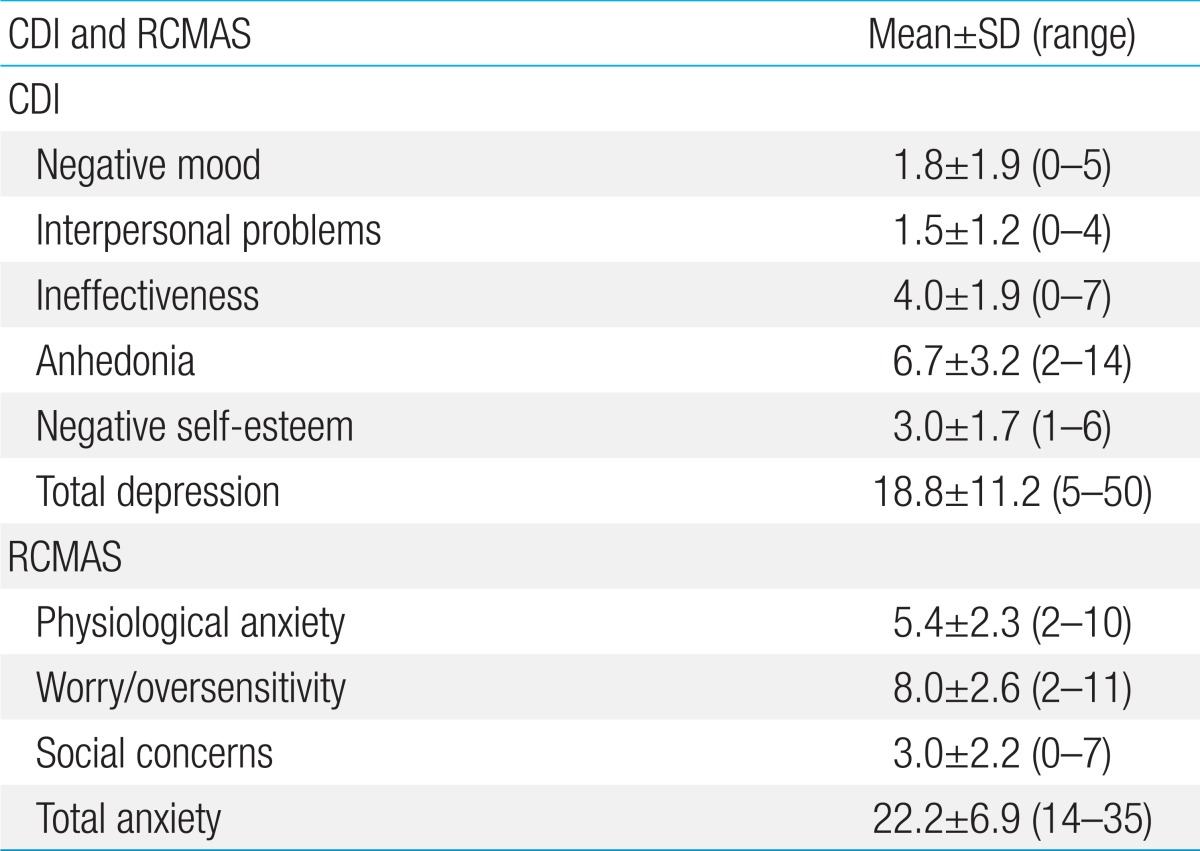
Thirteen patients exceeded the CDI clinically significant cutoff point for increased self-reported depression (CDI score>15). Mean total depression score was 18.8±11.2 and the highest score was 50. CDI scores in Anhedonia subclass were relatively high. Subscores of CDI and RCMAS are shown in Table 2.
Twenty patients exceeded the RCMAS clinically significant cutoff point for self-reported anxiety (RCMAS score>15). Mean total anxiety score was 22.2±6.9 and the RCMAS scores in the worry/oversensitivity subclass were relatively high.
There was no correlation between CDI or RCMAS total scores and headache frequency, duration, or intensity.
Patients in this study were assessed for behavioral and psychiatric disorders including depression, generalized anxiety disorder, bipolar disorder, somatoform disorder, emotional disorder and attention deficit/hyperactivity disorder (ADHD) (Table 3). Five patients (0.7%) had comorbid pure depression, one patient (0.14%) had comorbid pure anxiety disorder, and two patients (0.28%) had comorbid depression and anxiety disorder. Four patients (0.56%) were diagnosed with somatoform disorder and three patients (0.42%) were diagnosed with emotional disorder. Four patients (0.56%) were diagnosed with ADHD. A patient of referred to psychiatric clinic didn't have any other psychiatric disorders.
All patients received treatment for headaches. Of twenty patients that referred to a pediatric psychology clinic, ten patients were treated with headache medication and psychological treatment. Three patients were treated with headache medication, antipsychotic medication and psychological treatment. Two patients received only psychological treatment. One patient received a stimulant for ADHD.
Headache in children are sometimes somatic manifestations of psychiatric conditions, such as anxiety and depression6). Psychiatric problems have been investigated extensively in headache patients, especially in adult patients with migraine. However, children with headache have received less attention. A recent study investigating psychiatric comorbidity and suicide risk in adolescents with chronic daily headaches found that these adolescents are at high risk for suicide and have a high comorbidity of psychiatric disorders, particularly major depression and panic disorders7). In addition, several studies reported that psychiatric comorbidities could promote the transformations of episodic headaches into chronic symptoms, which in turn can make treatment more difficult and increase the likelihood of headache-related disabilities8,9,10). These findings will hopefully increase physician awareness of the importance of addressing psychiatric disorders in patients with headache.
Maizels et al.4) suggested that patients evaluated for headache should also be formally screened for depression and anxiety, at minimum. Smitherman et al.11) proposed a psychiatric screening which can be administered quickly at minimal costs. The most common and well-supported self-reporting method used to assess depression in children is the CDI and some researchers suggest that it may measure broader syndromes of general negative emotional distress. However, screening for depression alone is not sufficient and should be accompanied by screening for anxiety. The RCMAS subscales measure generalized anxiety disorder, somatic symptoms and depression. These tests require less time to complete and are suitable for use in the outpatient clinic.
In the headache outpatient clinic in the present study, CDI and RCMAS were used to detect depression and anxiety symptoms in children with primary headache. Most patients suffered from chronic headache before their first visit to the headache clinic (mean duration of headache: 11.5 months). Migraine was the most common type of headache. Mean total CDI and RCMAS scores of referred patients to psychiatric clinic were 18.8 and 22.2. These scores were higher than previously published scores from control group. Reale et al.12) reported that a normal control group had CDI score of 7.0±4.96, while Mazzone et al.13) reported that a normal control group had CDI score of 7.20±1.14.
In the present study, behavioral and psychiatric disorders including depression, generalized anxiety disorder, bipolar disorder, somatoform disorder, emotional disorder and ADHD were diagnosed by a pediatric psychologist (Table 3). Point seven present of the patients in this study had comorbid pure depression, 0.14% had comorbid pure anxiety disorder, and 0.28% had both comorbid both depression and anxiety disorder. Depression was the most common psychiatric disorder with 1.7% of subjects diagnosed as clinically depressed. Four patients (0.56%) were diagnosed with somatoform disorder and three (0.42%) were diagnosed with emotional disorder. Somatoform disorder in patients with headache has not been studied as extensively as depression or anxiety. In several previous studies, somatoform disorder with headache was found to be more prevalent than depression and anxiety. Okasha et al.14) found that 43% of patients with nonorganic headache had somatoform pain, while Nimnuan et al.15) reported that 27% of patients with headache had somatoform disorder. Children with multiple somatic complaints report symptoms of anxiety and depression more often than those with fewer or no somatic complaints. Most patients received treatment such as antipsychotic medication or psychotherapy for psychiatric disorders16).
Reale et al.12) reported that indices of behavioral and emotional difficulties, anxiety, depression and hyperactivity symptoms were elevated among clinically referred children suffering from migraine compared to their normal peers. However, most patients had behavioral and psychological scores within the normative, nonpathological range.
Previous studies have found that CDI scores correlated positively with headache frequency. In contrast, this study did not observe a correlation between CDI scores and headache frequency, duration, or severity. This result was contrary to previous studies in which headache frequency and duration were significantly associated with depression or anxiety. This discrepancy may be due to the relatively high CDI scores observed in patients in the present study compared to previous studies.
This study has several limitations. First, it is retrospective study. In addition, the screening test for psychiatric symptoms did not include assessment of behavioral problems. Last, this study didn't follow up referred patients' treatment results or effects.
In conclusion, patients with headache and comorbid psychiatric disorder can experience significantly decreased quality of life, poor prognoses, chronic diseases, and decreased response to treatment. Therefore, early recognition and management of psychiatric disorders is potentially of great value to headache patients. The authors recommended that all clinicians who treat headache patients screen for psychiatric disorders as part of their routine clinical evaluation. Screening should include symptoms for both anxiety and depression. A comprehensive evaluation of headache patients should incorporate formal and multidimensional psychiatric screening.
Acknowledgments
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2013R1A2A2A01014108).
References
1. Egger HL, Angold A, Costello EJ. Headaches and psychopathology in children and adolescents. J Am Acad Child Adolesc Psychiatry 1998;37:951–958.


3. Egermark-Eriksson I. Prevalence of headache in Swedish school children. A questionnaire survey. Acta Paediatr Scand 1982;71:135–140.


4. Maizels M, Smitherman TA, Penzien DB. A review of screening tools for psychiatric comorbidity in headache patients. Headache 2006;46(Suppl 3): S98–S109.


5. Gambini O, Barbieri V, Biagianti B, Scarone S. Consultation-liaison psychiatry for patients with headaches. Neurol Sci 2011;32(Suppl 1): S81–S83.


6. Venable VL, Carlson CR, Wilson J. The role of anger and depression in recurrent headache. Headache 2001;41:21–30.


7. Wang SJ, Juang KD, Fuh JL, Lu SR. Psychiatric comorbidity and suicide risk in adolescents with chronic daily headache. Neurology 2007;68:1468–1473.


8. Jette N, Patten S, Williams J, Becker W, Wiebe S. Comorbidity of migraine and psychiatric disorders: a national population-based study. Headache 2008;48:501–516.


10. Scher AI, Lipton RB, Stewart W. Risk factors for chronic daily headache. Curr Pain Headache Rep 2002;6:486–491.


11. Smitherman TA, Maizels M, Penzien DB. Headache chronification: screening and behavioral management of comorbid depressive and anxiety disorders. Headache 2008;48:45–50.


12. Reale L, Guarnera M, Grillo C, Maiolino L, Ruta L, Mazzone L. Psychological assessment in children and adolescents with Benign Paroxysmal Vertigo. Brain Dev 2011;33:125–130.


13. Mazzone L, Vitiello B, Incorpora G, Mazzone D. Behavioural and temperamental characteristics of children and adolescents suffering from primary headache. Cephalalgia 2006;26:194–201.


14. Okasha A, Ismail MK, Khalil AH, el Fiki R, Soliman A, Okasha T. A psychiatric study of nonorganic chronic headache patients. Psychosomatics 1999;40:233–238.






 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


