Article Contents
| Korean J Pediatr > Volume 53(6); 2010 |
Abstract
Purpose
To determine the clinical manifestations and outcomes of patients with tracheoesophageal fistula (TEF) and esophageal atresia (EA) born at a single neonatal intensive care unit.
Methods
A retrospective analysis was conducted for 97 patients with confirmed TEF and EA who were admitted to the neonatal intensive care unit between 1990 and 2007.
Results
The rate of prenatal diagnosis was 12%. The average gestational age and birth weight were 37+2 weeks and 2.5┬▒0.7 kg, respectively. Thirty-one infants were born prematurely (32%). Type C was the most common. The mean gap between the proximal and distal esophagus was 2 cm. Esophago-esophagostomy was performed in 72 patients at a mean age of 4 days after birth; gastrostomy or duodenostomy were performed in 8 patients. Forty patients exhibited vertebral, anorectal, cardiac, tracheoesophageal, renal, limb (VACTERL) association with at least 2 combined anomalies, and cardiac anomaly was the most common. The most common post-operative complications were esophageal stricture followed by gastroesophageal reflux. Balloon dilatation was performed for 1.3 times in 26 patients at a mean age of 3 months. The mortality and morbidity rates were 24% and 67%, respectively, and the most common cause of death was sepsis. The weight of approximately 40% patients was below the 10th percentile at 2 years of age.
The reported incidence of tracheoesophageal fistula (TEF)/esophageal atresia (EA) is roughly 1-2 per 5,000 live births and can be seen regularly in most tertiary neonatal units that care for high-risk infants1). Since the first successful corrective surgery in 1939, the majority of neonates with TEF/EA can expect a satisfactory outcome due to the progress in surgery techniques, neonatal intensive care, and neonatal anesthesia over the past 60 years2, 3).
Herein, we report the clinical characteristics, combined anomalies of the TEF/EA, risk factors associated with mortality, and long-term morbidities of TEF/EA, according to Gross's4) anatomic classification, observed in a single neonatal intensive care unit over the past 18 years.
The subjects included those newly born infants with TEF/EA admitted from April 1994 to February 2007 who underwent corrective surgery at the neonatal intensive care unit of the Asan Medical Center. Patients transferred from other hospitals with suspected TEF/EA and whose diagnosis was later confirmed were included; however, patients transferred to the unit after corrective surgery was performed were excluded.
The medical records of 97 infants satisfying the above criteria were retrospectively reviewed for various prenatal and postnatal clinical characteristics, operative findings, combined anomalies, morbidities including esophageal strictures, gastroesophageal reflux, and weight gain for the 2-year period after birth. Various factors were reviewed to analyze the risk factors associated with the mortality of TEF/EF.
VACTERL association was defined if the patient has 2 or more anomalies of the vertebral, anorectal, cardiac (excluding patent ductus arteriosus, patent foramen ovale), renal/genitourinary, and limb systems.
Multiple logistic regression analyses were performed on univariate variables, including hospital days, gestational age, birth weight, Apgar score, maternal age, polyhydramnios, type of TEF/EA, VACTERL association, ventilator days, time of operation, esophageal stricture requiring esophageal balloon dilatation under fluoroscopic guidance, and tracheostomy to seek risk factors associated with mortality. All data were considered statistically significant if P<0.05. SAS 9.1 (2003 version; SAS Institute Inc.; Cary, NC) was used.
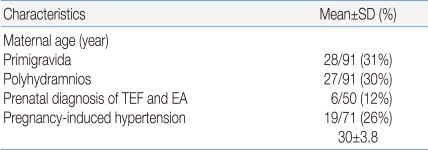
The average age (┬▒standard deviation) of mothers who gave birth to newborns with TEF/EA was 30┬▒3.8 years. Of the 91 (30%) mothers, 27 had , and prenatal diagnosis was suspected in only 6/50 (12%) (Table 1).
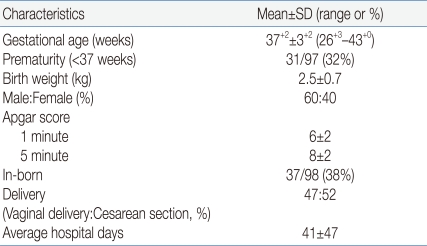
The average gestational age of newborns with TEF/EA was 37+2 weeks, and the percentage of premature infants was 32%. The average birth weight was 2.5┬▒0.7 kg, and more males than females were diagnosed. The percentage of in-born newborns was only 38%. There was a slight preponderance of babies born via cesarean section, and the average length of hospitalization was 41┬▒47 days (Table 2).
Of those newborns who underwent chromosomal analysis, 2 out of 19 had abnormal results: Edward syndrome (47,XX,+18) in 1 and DiGeorge syndrome (46,XX,t(4;5)(q35;q33.1) in another.
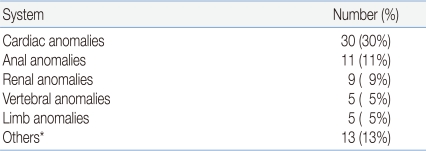
A total of 51% of the newborns had at least one congenital anomaly other than TEF/EA, and 41% of the anomalies were within the constellation of defects of VACTERL association. In order of approximate frequency, the affected organ systems most commonly associated with TEF/EA were cardiovascular, anorectal, genitourinary and skeletal. The most common congenital heart disease was tetralogy of Fallot (43%) followed by ventricular septal defect (20%), double outlet right ventricle associated with pulmonary atresia/pulmonary stenosis (13%), dextrocardia (10%), aortic stenosis and ventricular septal defect (3%), atrial and ventricular septal defect (3%), double outlet right ventricle and functional single ventricle (3%), and mitral atresia (3%). Of those with imperforate anus, 55% had high type.
The renal anomalies in the order of frequency were unilateral renal agenesis, vesicoureteral obstruction, horseshoe kidney, crossed renal ectopia, hydronephrosis, and multicystic dysplastic kidney. The vertebral anomalies, 5% of the total anomalies, included polydactyly, syndactyly, and club hand (Table 3).
Thirteen out of 40 neonates with VACTERL association had other congenital anomalies, including single umbilical artery (5 cases) followed by cleft palate (3 cases), craniosynostosis (1 case), agenesis of eyes and nose (1 case), small mandible (1 case), and tongue tie (1 case).
The gastrointestinal anomalies other than anorectal defects included duodenal obstruction, hypertrophic pyloric stenosis, malrotation, and biliary atresia. Congenital diaphragmatic hernia, subglottic stenosis, congenital dysplasia of hip, and hypoplastic thymus in a patient with DiGeorge syndrome were also observed in small numbers.
Surgical intervention was performed, on average, the 4th day after birth on 81 neonates. Parents of 16 neonates refused further treatment due to the multiple congenital anomalies found. Immediate primary repair was possible in 72 cases (88%), and staged repair was performed in 8 cases (9%) after gastrostomy or duodenostomy due to the long esophageal gap. Simple ligation of fistula was done in 1 case (1%). The average length from the proximal to the distal esophageal pouch was 2 cm (range: 1.4-3 cm).
Out of 8 patients who underwent gastrostomy or duodenostomy, 4 patients expired preoperatively due to sepsis or respiratory failure from pneumonia before definitive corrective surgery. Two patients born in 1991 had esophageal replacement surgery with the colon at 14 months and 17 months of age, and 1 patient born in 2000 underwent delayed primary repair of the esophagus at 19 months of age.
The most common anatomical variant was type C, found in 71 patients (91%), followed by type A in 2 patients (2%), type E in 3 cases (4%), and type B or D in 1 case (1%). The average length of ventilation was 9.6 days (range: 1-106 days).
Among the 81 patients who underwent surgical corrections, contrast esophagogram was performed using barium on an average of 25 days after the surgery. Forty-seven patients (64%), 29 patients (39%), and 9 patients (12%) showed anastomotic strictures, reflux, and leaks, respectively. Of the 47 patients, 26 were demonstrated to have strictures on average 3 months after the surgery and required balloon dilatation an average of 1.3 times per patient. Recurrent fistulas occurred in 2 patients; primary surgical closure was required in 1, and spontaneous regression of fistula occurred in the other.
The study period was divided into 2 periods. The mortality rates for the periods 1990 to 1999 and 2000 to 2007 were 39% and 23%, respectively. Parents of 4 patients refused further treatment due to multiple congenital anomalies, resulting in 24 out of 39 patients surviving during the first study period in comparison to 2 patients whose parents refused treatment for the same reasons as in the first study period and 2 patients who were lost to follow-up, resulting in 45 out of 58 patients surviving during the second study period (Fig. 1).
Excluding those patients who did not get treatment and were lost to follow-up, the overall mortality rate was 20% (20/97 patients). The most common etiology causing death was sepsis followed by respiratory failure, subendocarditis, congestive heart failure, gastrointestinal hemorrhage, liver cirrhosis, and gastric perforation. Out of the 40 patients with VACTERL association, 30% (12/40 patients) died; the mortality rate was higher than the overall mortality rate. The mortality rate was 16% (5/30 patients) for those who had cardiac anomalies among patients with VACTERL association.
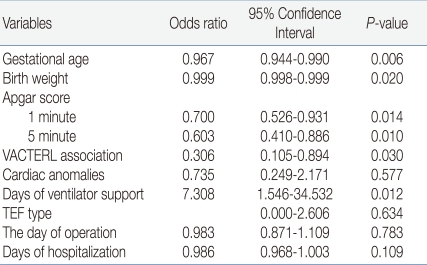
To assess the risk factors associated with mortality, multiple regression analyses of aforementioned univariate variables were conducted, and gestational age, birth weight, 1-minute and 5-minute Apgar scores, VACTERL association, and ventilator days were significantly associated with mortality (Table 4).
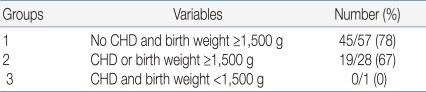
To delineate the effect of congenital cardiac anomaly and birth weight with prognosis, birth weight was stratified into 3 groups with or without associated cardiac anomalies: Out of 57, 45 infants survived. Of the 28 infants with cardiac anomalies and birth weight above 1,500 g, 67% survived; in contrast, 78% of those without cardiac anomalies and birth weight above 1,500 g survived (Table 5).
Excluding those who were lost to follow-up, a total of 72 patients were evaluated for respiratory and gastrointestinal morbidities. The morbidities included laryngomalacia (2%), cricopharyngeal incoordination (4%), recurrent pneumonia (4%), tracheostomy (5%), esophageal stricture, dysphagia (65%), and gastroenteral reflux (38%).
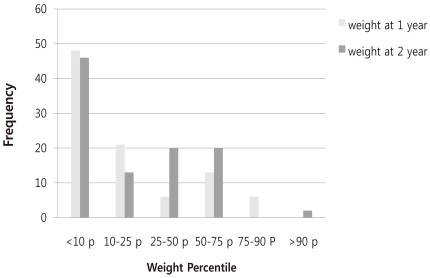
The weight gain at 1 year and 2 years of the patients who survived showed that 48% and 19% of the infants were below the 10th percentile and the 3rd percentile, respectively, at 1 year in contrast to 45% and 19%, respectively, at 2 years old (Fig. 2).
Of the 11 infants whose birth weight was below the 10th mesenchymal growth can stretch and disrupt the esophagus, creating esophageal atresia6).
Unlike other congenital anomalous disease, the prenatal detection rate of TEF is low: Sparey et al and De Vigan et al7, 8) reported that prenatal detection was possible in 9.2% and 24% of cases, respectively. The prenatal detection rate in our institution was 12%, a result reflecting more aggressive attempts to conduct prenatal diagnosis during the second phase of the study period. The positive predictive value of both polyhydramnios and a small or absent stomach bubble has been reported to be only 56%, making prenatal diagnosis even more difficult9).
The ratio of males to females was 6:4 in our study, a result similar to the incidence reported by Waterson et al10). Congenital malformations, including TEF/EA, are known to occur more commonly in twins. Mastroiacovo et al11) found that of 92 malformations studied, 39 malformations including TEF/EF were more common in twins than in singletons. The authors reported that the relative risk for TEF/EF in twins compared with singletons was 2.56 (95% confidence interval 2.01-3.25). In our series, the frequency of TEF/EA among twinning was 5%, and of interest, TEF/EF was observed in both fraternal twins.
The incidence of other anomalies associated with TEF/EA is reported to be 30-60%10, 12, 13), a result similar to our study of 52% where one or more anomalies was found. The most common anomaly was cardiovascular (35%) followed by genitourinary (24%), gastrointestinal (24%), musculoskeletal (13%), and neurologic (10%). An abnormal chromosomal study was found in 10% in our study, a result similar to other reports7, 14, 15). The most commonly occurring congenital heart disease as reported by Choi et al3), in order of frequency, was ventricular septal defect, patent ductus arteriosus, atrial septal defect, aortic stenosis, tetralogy of Fallot, truncus, and transposition of great vessels, whereas our finding suggested that tetralogy of Fallot was the most commonly found congenital heart disease. About 1/3 of patients presenting with a gap of more than 2 cm between the proximal and distal esophagus were reported to result in anastomotic leak, recurrence of TEF, gastroesophageal reflux, and anastomotic stricture as postoperative complications3, 16). An ultra-long gap of more than 3 cm was more frequently observed in patients with vascular ring, TEF with proximal esophageal atresia, or esophageal atresia without TEF3, 16, 17) in which frequent postoperative complications, including respiratory compromise, dysphagia, and growth failure18), are known to occur. This was also true in our study of 7 infants with an ultra-long gap; 4 infants died, 2 infants showed failure to thrive, and only 1 infant showed normal growth for age.
The 20% mortality rate in our study is similar to the mortality rates reported by others of 10-30%12, 13, 19). Variables, including gestational age, birth weight, 1-minute and 5-minute Apgar scores, VACTERL association, and duration of ventilator days, seemed to affect the mortality rate in patients with TEF/EA, a finding different from that reported by Choi et al3). Nevertheless, both reports are in agreement in that prematurity is an important variable influencing survival: a survival rate of 87% among full-term infants in comparison to a 62% survival rate among preterm infants. Boyle et al17) and Spitz et al20) reported that the survival of full-term infants with TEF/EA without associated anomaly was 95-100%.
In contrast to reports by Sparey et al7) and Engum et al21), our study showed that gastrointestinal complications were more frequently observed than respiratory-related complications. Esophageal stricture and gastroesophageal reflux were observed in 65% and 39%, respectively, of our study population.
The upper gastrointestinal morbidity and anthropometric data collected by Chetcuti and Phelan22) in 334 patients aged 1 to 37 years with repaired TEF/EA showed that 67% required hospitalization with esophageal complications and half underwent one or more surgical procedures. More importantly, the patients' median weight centile was the 25th. Such findings and a report by Kim et al23) are in accordance with our report in which the percentage of infants whose weight remained below the 10th percentile at 1 year old and 2 years old was 48% and 45%, respectively.
In conclusion, the overall mortality rate (20%) and morbidity rate (67%) of infants born with TEF/EA are high due to the associated anomalies and gastroesophageal and respiratory complications during infancy. Longer follow-up into childhood and adulthood is needed in the future as the long-term outcome of the majority of adults who experienced a difficult initial period is reported to be excellent, and they enjoy a normal lifestyle22).
References
1. Depaepe A, Dolk H, Lechat MF. The epidemiology of tracheooesophageal fistula and oesophageal atresia in Europe. EUROCAT Working Group. Arch Dis Child 1993;68:743ŌĆō748.



3. Choi PJ, Jun HJ, Lee YH, Jo KJ, Sung SC, Woo CS. Surgical treatment of the congenital esophageal atresia. Korean J Thorac Cardiovasc Surg 1999;32:567ŌĆō572.
4. Gross R. The surgery of infancy and childhood. 1957;Philadelphia: WB Saunders Co.
5. Kovesi T, Rubin S. Long-term complications of congenital esophageal atresia and/or tracheoesophageal fistula. Chest 2004;126:915ŌĆō925.


6. Emery JL, Haddadin AJ. Squamous epithelium in respiratory tract of children with tracheo-oesophageal fistula. Arch Dis Child 1971;46:236ŌĆō242.



7. Sparey C, Jawaheer G, Barrett AM, Robson SC. Esophageal atresia in the Northern Region Congenital Anomaly Survey, 1985-1997: prenatal diagnosis and outcome. Am J Obstet Gynecol 2000;182:427ŌĆō431.


8. De Vigan C, Goujard J, Vodovar V, Uzan S. Management of the fetus with a correctable malformation in Paris maternity units: evolution 1985-1994. Fetal Diagn Ther 1997;12:216ŌĆō220.


9. Achildi O, Grewal H. Congenital anomalies of the esophagus. Otolaryngol Clin North Am 2007;40:219ŌĆō244.


10. Waterston DJ, Carter RE, Aberdeen E. Oesophageal atresia: tracheooesophageal fistula. A study of survival in 218 infants. Lancet 1962;1:819ŌĆō822.

11. Mastroiacovo P, Castilla EE, Arpino C, Botting B, Cocchi G, Goujard J, et al. Congenital malformations in twins: an international study. Am J Med Genet 1999;83:117ŌĆō124.


12. Bishop PJ, Klein MD, Philippart AI, Hixson DS, Hertzler JH. Transpleural repair of esophageal atresia without a primary gastrostomy: 240 patients treated between 1951 and 1983. J Pediatr Surg 1985;20:823ŌĆō828.


13. Louhimo I, Lindahl H. Esophageal atresia: primary results of 500 consecutively treated patients. J Pediatr Surg 1983;18:217ŌĆō229.


14. Ein SH, Shandling B, Wesson D, Filler RM. Esophageal atresia with distal tracheoesophageal fistula: associated anomalies and prognosis in the 1980s. J Pediatr Surg 1989;24:1055ŌĆō1059.


15. Engum SA, Grosfeld JL, West KW, Rescorla FJ, Scherer LR 3rd. Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over two decades. Arch Surg 1995;130:502ŌĆō508.


16. Hagberg S, Rubenson A, Sillen U, Werkmaster K. Management of long-gap esophagus: experience with end-to-end anastomosis under maximal tension. Prog Pediatr Surg 1986;19:88ŌĆō92.


17. Boyle EM, Irwin ED, Foker JE. Primary repair of ultra-long-gap esophageal atresia: results without a lengthening procedure. Ann Thorac Surg 1994;57:576ŌĆō579.


18. Hands LJ, Dudley NE. A comparison between gap-length and Waterston classification as guides to mortality and morbidity after surgery for esophageal atresia. J Pediatr Surg 1986;21:404ŌĆō406.


19. Kim SC, Kim DY, Kim EA, Kim KS, Pi SY, Kim IK. Clinical experience of esophageal atresia. J Korean Assoc Pediatr Surg 2003;9:6ŌĆō11.

20. Spitz L, Kiely E, Brereton RJ. Esophageal atresia: five-year experience with 148 cases. J Pediatr Surg 1987;22:103ŌĆō108.


21. Engum SA, Grosfeld JL, West KW, Rescorla FJ, Scherer LR 3rd. Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over two decades. Arch Surg 1995;130:502ŌĆō508. discussion 8-9.


22. Chetcuti P, Phelan PD. Gastrointestinal morbidity and growth after repair of oesophageal atresia and tracheo-oesophageal fistula. Arch Dis Child 1993;68:163ŌĆō166.



23. Kim JY, Choe BH, Ko JS, Park KW, Seo JK. Motor dysfunction of the esophagus after repair of esophageal atresia and tracheoesophageal fistula. Korean J Gastrointest Motil 2001;7:21ŌĆō28.
Fig.┬Ā1
Comparison between mortality rates of 1990-1999 and 2000-2007. The mortality rate decreased during 2000-2007 as compared to that during 1990-1999. Abbreviation: AMA, against medical advice.
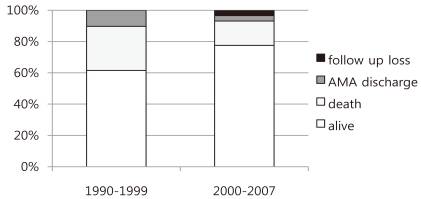
Fig.┬Ā2
Comparison between weights at 1 year and 2 years. The weight of patients at 2 years increased as compared to that of patients at 1 year. However, more than 40% of the patients still weighed below the 10th percentile.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


