Article Contents
| Clin Exp Pediatr > Volume 66(3); 2023 |
|
Abstract
Chronic liver disease incidence is increasing among children worldwide due to a multitude of epidemiological changes. Most of these chronic insults to the pediatric liver progress to fibrosis and cirrhosis to different degrees. Liver and immune physiology differs significantly in children from adults. Because most of pediatric liver diseases have no definitive therapy, a better understanding of population and disease-specific fibrogenesis is mandatory. Furthermore, fibrosis development has prognostic significance and often guide treatment. Evaluation of liver fibrosis continues to rely on the gold-standard liver biopsy. However, many high-quality studies put forward the high diagnostic accuracy of numerous diagnostic modalities in this setting. Herein, we summarize and discuss the recent literature on fibrogenesis with an emphasis on pediatric physiology along with a detailed outline of disease-specific signatures, noninvasive diagnostic modalities, and the potential for antifibrotic therapies.
Graphical abstract.
HSC, hepatic stellate cell; ECM, excess extracellular matrix; ROS, reactive oxygen species; ER, endoplasmic reticulum; IFALD, intestinal failure-associated liver disease; NAFLD-NASH, nonalcoholic fatty liver disease-nonalcoholic steatohepatitis; AIH, autoimmune hepatitis; CHF, congestive heart failure; METAVIR, metaanalysis of histological data in viral hepatitis; VCTE, vibration-controlled transient elastography; USG, ultrasonography; MR, magnetic resonance; FXR, farnesoid X receptor; NK, natural killer; TIMP, tissue inhibitors for metalloproteinases.
The incidence of chronic liver disease (CLD) is increasing among children worldwide owing to a multitude of epidemiological changes, such as the opioid epidemic for hepatitis C infection and obesity epidemic for nonalcoholic fatty liver disease (NAFLD) [1]. The overall incidence of liver disease in infants is 1 in 2,500, while in 2021, children represented 13% of all liver transplantations (LTs) in the US [2,3]. CLDs in pediatrics are heterogeneous and span a wide range of pathologies ranging from congenital or metabolic disorders to autoimmune diseases and viral diseases. Most chronic insults to the pediatric liver have the potential to progress to fibrosis and cirrhosis to different degrees.
The pathophysiology of fibrosis is a well-researched area with significant focus on novel biomarkers and antifibrotic treatments, especially in the adult population. Little is known about how this pathophysiology differs in the pediatric population, which has a unique hepatic and immune milieu. Moreover, certain pathologies in the pediatric population are distinct and characterized by different rates of fibrosis progression. For instance, fibrosis requires months to occur in all patients but neonates [4].
Depending on the etiology, follow-up of liver fibrosis is often required to define treatment goals. However, liver biopsy remains the gold-standard tool for this purpose despite its limitations such as invasiveness, complications, and inadequate sampling. Therefore, research has focused on noninvasive modalities and potential predictive biomarkers, and a review of these efforts in the pediatric population is required.
This article will outline the distinctions between adult and pediatric liver fibrosis with specific emphasis on pathophysiology, individual pediatric diseases, diagnostic modalities, and the ongoing search for therapeutic strategies for liver fibrosis.
Liver fibrosis involves replacement of the hepatic parenchyma by excess extracellular matrix (ECM) as part of a wound healing response to chronic hepatic or bile duct injury [5]. The deposition of fibrillar collagen (i.e., collagen I, collagen III, and fibronectin) and unusual ECM proteins (e.g., chondroitin-sulfate rich proteoglycans) results in altered liver microarchitecture. These structural changes impede the bidirectional flow of plasma between the sinusoidal lumen and hepatocytes, resulting in further hepatic compromise [6].
In the liver, the major event that drives fibrogenesis is the activation and differentiation of hepatic stellate cells (HSCs) into α-smooth muscle actin (α-SMA)–positive myofibroblasts (MFs) with high profibrogenic capacity. In the normal liver, HSCs reside in the subendothelial space of Disse, the interface between hepatocytes and sinusoids, and store fat and vitamin A [7]. In a 2013 monumental study, HSCs were the major source of MFs in HSC-marked Cre-transgenic mouse models of toxic, cholestatic, and fatty liver disease [8]. In addition to the central role of HSC in fibrosis, recent studies revealed that multiple molecular and cellular processes are involved in this dynamic process (Fig. 1). Although experimental data are scarce, the pathophysiological steps outlined above may differ in multiple ways in the pediatric population (Fig. 2).
Pediatric liver disease spans a large spectrum of diseases with heterogeneous pathophysiology, age range, and course. Liver diseases are hereditary except for NAFLD, viral hepatitis, primary sclerosing cholangitis (PSC), and autoimmune liver disease. Accordingly, the potential of these diseases to lead to fibrosis is different. Biliary atresia (BA), intestinal failure-associated liver disease (IFALD), and certain metabolic/genetic liver diseases characteristically begin in the neonatal period and manifest significant fibrosis early. Others, such as Alagille syndrome and autosomal recessive polycystic kidney disease, despite having a neonatal or even prenatal onset, present with fibrosis in older children. Table 1 summarizes the characteristics of chronic pediatric liver pathologies associated with fibrosis [6].
BA is a progressive fibroinflammatory disease involving a segment or the entire extrahepatic biliary tree that leads to obliteration of the affected bile ducts within the first 3 months of life. To date, the exact pathophysiology of BA has remained elusive with a focus on environmental insults, immunologic dysregulation, genetic susceptibility, and developmental defects. The current hypothesis endorses a viral insult, leading to overactivation of the immune system. Fibrosis in BA is unique in that it progresses rapidly, leading to cirrhosis within a few weeks of birth in untreated cases. Kasai portoenterostomy (KPE) bypasses the atretic extrahepatic bile ducts and restores bile flow. The therapeutic outcome of KPE was evaluated using serum bilirubin levels at 6 months postoperative. Despite a good clinical response to KPE, liver fibrosis in BA often progresses to cirrhosis, requiring LT. In different series published worldwide, the rate of needing LT after KPE was 45%–70% at 5 years. Research has focused on identifying prognostic indicators in the post-KPE setting to predict progression to fibrosis and cirrhosis [9,10].
PSC is a chronic fibroinflammatory disorder of the intrahepatic and/or extrahepatic bile ducts of unknown etiology. The development of fibrosis is significant in pediatric PSC [11-16]. Despite the inconspicuous symptoms at presentation, such as fatigue and favorable magnetic resonance cholangiopancreatography scores, the majority of pediatric patients have significant fibrosis in the initial liver biopsy [17,18]. Around 1%–2% of adults, but 17%–30% of children progress to advanced liver disease and require LT each year [12,19]. In a large multicenter study of 781 children, Deneau et al. [11] found that a high fibrosis scoring aspartate transaminase (AST) to platelet ratio index (APRI) portends a poor prognosis.
No treatment options to date, such as oral vancomycin or ursodeoxycholic acid, are associated with improved fibrosis in pediatric PSC [20,21]. Haisma et al. [22] performed a genome-wide association study of 29 patient-parent trios with PSC onset at ≤12 years of age. They found pathogenic variants in 22 of 29 of patients and that some of the genes were involved in transmembrane transport, adaptive and innate immunity, and epithelial barrier function. On the other hand, adult genome studies identified most adult-onset susceptibility genes to the human leukocyte antigen complex II locus [23,24]. Therefore, pediatric PSC may represent a heterogeneous disease characterized by differing mechanisms and potential for fibrosis that may benefit from individualized treatment.
Alagille syndrome is a multisystem disorder of morphogenesis that characteristically involves cholestasis, heart murmur, structural heart disease, dysmorphic facial features, vertebral anomalies, and optical findings. Through a mutation in the JAG1 gene on chromosome 20, commonly NOTCH2, the Notch signaling pathway is perturbed, resulting in complex developmental manifestations [25]. Liver involvement in Alagille syndrome is characterized by bile duct paucity, cholestasis, and fibrosis. Although the liver disease may improve with age, 43.5%–76% of patients reportedly require LT by adulthood [26-28].
Defective Notch signaling associated with Alagille syndrome has guided our understanding of biliary fibrosis. Upon injury, hepatic progenitor cells (HPCs) are activated and have the capacity to differentiate into hepatocyte as well as biliary epithelial cells in hepatocellular and biliary injury, respectively. Jagged-1 expressing portal MFs mediate the differentiation of HPCs upstream of Notch signaling. The outcome of Alagille syndrome is a scarcity of reactive ductular cells, resulting in thinner portal septa and an abundance of intermediate hepatic-biliary cells that promote intralobular chicken wire fibrosis [29,30].
Most children acquire hepatitis B virus (HBV) and/or hepatitis C virus (HCV) infections in infancy, with 90% and 60% developing chronic infections, respectively [31,32]. Overall, chronic HCV infection in children follows an indolent course with low-level fibrosis. In 2 cohorts of 121 and 332 children, only 2 and 6 children developed cirrhosis in longitudinal follow-up, respectively [33,34]. Despite vaccination, HPV remains an important source of mortality and morbidity in children in the United States. In a study of histological specimens collected from 134 children, fibrosis and cirrhosis were present in 82% and 4%, respectively. In another study of 292 HBV-infected children, cirrhosis occurred in 3% at a median of 4 years of age [35,36].
In chronic HBV, Łotowska and Lebensztejn [37] found a positive correlation between the number of SMA-positive HSCs and fibrosis stage. The same group performed an ultrastructural phenotype analysis of chronic HBV biopsies and documented shifts in 2 cell types in children with advanced fibrosis: quiescent HSCs were replaced with transitional and MF-like HSCs and damaged liver progenitor cells in close proximity to the HSCs [38-40]. Close monitoring of fibrosis progression guides clinical decisions to begin antiviral therapy in these patients to prevent ongoing fibrosis [41].
Autoimmune hepatitis (AIH) is a chronic inflammatory disease of the liver characterized by hypergammaglobulinemia and autoantibody positivity. AIH is an important consideration in childhood liver fibrosis since one-third of patients present with cirrhosis and its complications [42,43]. Maia et al. [44] performed immunohistochemical examinations of pediatric AIH liver biopsies and noted that the activation of HSC populations decreased significantly following therapy. Studies involving follow-up biopsies in 16 and 13 pediatric patients with AIH demonstrated regression of fibrosis over 6–12 months [45,46].
NAFLD is a disease spectrum that ranges from hepatocyte steatosis to nonalcoholic steatohepatitis (NASH) to fibrosis and ultimately cirrhosis [47]. Fibrosis in NAFLD-NASH is perhaps the most studied pathophysiology in terms of mechanisms, diagnostics, and therapeutics. Atsawarungruangkit et al. [48] performed transient elastography-based screenings of 740 US adolescents embedded within the 2017–2018 National Health and Nutrition Examination Survey and identified advanced fibrosis secondary to NAFLD in 2.84%. According to an evaluation of liver biopsies from 100 children with NAFLD, 2 phenotypes of pediatric NASH exist: type I, with lobular inflammation and perisinusoidal fibrosis (17% of biopsies); and type II, with portal inflammation and fibrosis (51% of biopsies) [49]. Notably, children with the type II phenotype had more significant fibrosis.
The factors involved in driving the progression of NAFLD to fibrosis have been extensively evaluated. The 2 consistent risk factors for fibrosis development are metabolic syndrome and waist circumference [50-52]. Genetic variation is another source of wide study. Recently, Tao et al. performed a meta-analysis of 42 studies (>1 million participants), including 10 pediatric studies, to assess the role of rs641738C>T in MBOAT7. Although the variant was associated with advanced fibrosis on biopsy, its functional implications remain unclear. Another widely established variant is the rs738409 polymorphism in PNPLA3/adiponutrin. A meta-analysis of 5 studies with histological fibrosis assessments showed a significant association between advanced fibrosis and the variant [53]. In a study of 54 patients with NAFLD, those carrying the PNPLA3 variant had more periportal/portal fibrosis, hepatic progenitor cell activation, and serum oxidative stress [54]. Whether these findings can be applied to other etiologies could pose a worthwhile research question.
Environmental influences, such as dysbiosis and in utero exposure to a maternal Western diet, are related not only to NAFLD, but also to early liver fibrosis. NASH et al. recently demonstrated that nonhuman primate fetuses exposed to a maternal Western-style diet displayed increased fibrillar collagen deposition in the liver periportal region with localized HSC and MF activation. In a similar model, Friedman et al. [55] prevented collagen fibril formation in the offspring of mice fed a Westernstyle diet through a potent antioxidant, pyrroloquinoline quinone, which reversed macrophage metabolic programming from oxidative to glycolytic pathways and improved gut tight junction expression. Therefore, dietary modulation may be an important intervention for all patients with liver diseases.
IFALD encompasses a spectrum of liver diseases, including steatosis, cholestasis, and fibrosis, in patients with intestinal failure and long-term use of parenteral nutrition (PN) [56]. It reportedly affects 22%–30% of such children according to clinical diagnoses [57,58]. However, in a recent study, surveillance biopsies in children receiving PN revealed an abnormal histology in 94% and 77% during and after PN, respectively. Of them, 88% and 64% had portal/periportal fibrosis [59]. The causes of IFALD are still being delineated with potential culprits involving plant sterols in PN lipid emulsion, gut dysbiosis, impaired barrier function, and episodes of sepsis. The fibrotic liver milieu in IFALD, even after weaning from PN, has been characterized by α-SMA+HSCs, increased collagen expression, and profibrotic/inflammatory cytokines, such as interleukin (IL)1a, IL1b, epithelial growth factor, adhesion molecule integrin-β6, and matrix metalloprotein (MMP)9 [60-62].
Congenital hepatic fibrosis is mostly associated with autosomal recessive polycystic kidney disease and a PKHD1 gene mutation that encodes for the transmembrane protein fibrocystin/polyductin, is localized to cilia, and is involved in the development of the renal collecting duct and biliary system [63]. Therefore, the characteristic pathological lesion in the liver is a ductal plate malformation, in which irregular biliary channels persist around the portal tracts [64]. Fibrosis can be severe, forming thick white bands of fibrous tissue across hepatocyte cell islands [65]. Mutation type affecting the PKHD1 gene determines the severity of associated polycystic kidney disease but not congenital hepatic fibrosis [66]. LT outcomes are promising, with good kidney and liver function, even in related living donor LT [67,68].
Cystic fibrosis (CF) liver disease (CFLD), which develops in 5–10% of patients with CF, is characterized by progressive hepatobiliary fibrosis. In a recent cohort study of 3,328 CF patients, of whom 32.2% and 10% developed CFLD and severe CFLD by 30 years of age, respectively [69]. Lewindon et al. [70] longitudinally followed 41 patients with CF and found that fibrosis at baseline biopsies, but not clinical or imaging abnormalities, heralded the development of clinically significant CFLD/portal hypertension.
However, the patchy nature of disease sampling may be inadequate for quantifying fibrosis. For the noninvasive diagnosis of liver fibrosis, Pereira et al. [71] correlated various serum markers of fibrosis in a cohort of 36 children with CFLD. Lewindon et al. [72] investigated the diagnostic performance of vibration-controlled transient elastography (VCTE) and APRI/Fibrosis-4 (FIB-4) Index for staging fibrosis in 27 and 51 children, respectively. In these studies, VCTE (area under the receiver operating characteristic curve [AUROC], 0.89), APRI (AUROC, 0.83), and prolyl hydroxylase (AUROC, 0.81) were superior to others in determining a meta-analysis of histological data in viral hepatitis (METAVIR) score ≥ F3 and Scheuer stage ≥2 fibrosis [72,73]. Future studies should provide clinical benefits to this patient group owing to the silent progression of fibrosis.
Fontan-associated liver disease (FALD) represents a congestive hepatopathy related to elevated central venous pressures that follow the Fontan operation and final-stage surgical palliation for univentricular physiology through complete cavopulmonary shunt creation [74]. According to studies on surveillance biopsies, nearly all biopsied patients develop significant fibrosis during adolescence [75]. Among our cohort of Fontan patients, FALD was detected in 87.5%. Liver stiffness showed a significant positive correlation with post-Fontan duration (P<0.05, r=0.550) and the FIB-4 index (r=0.7, P<0.05) but not with APRI. Splenomegaly (P<0.01, r=0.669), APRI (P<0.01, r=0.767), and FIB-4 index (P<0.01, r=0.922) were all correlated with postFontan duration, implying the importance of universal screening depending on the timing after surgery.
Owing to the improvements in post-LT care, the 10-year patient and graft survival rates in pediatric LT are 83% and 73%, respectively [76]. However, progressive liver fibrosis is among the most common causes of liver allograft failure in the pediatric group, reaching as high as 69%–97% according to different centers [77-81]. Both alloimmune inflammation and biliary outflow obstruction contribute to ongoing fibrosis [5]. Alterations in the gut microbiome and intestinal permeability are potential contributors through pathogen-associated molecular pattern translocation and pattern recognition receptor activation, abnormal bile acid metabolism, and short-chain fatty acid imbalances [82]. According to sequential allograft biopsies in the study by Varma et al. [83], the histological lesion begins with portal inflammation and progresses to periportal fibrosis, followed by extension to adjacent portal fields. Small longitudinal studies have shown that intensification of immunosuppression after histological diagnosis of inflammation and fibrosis leads to a reduction in fibrosis scores [80,84]. To date, studies investigating noninvasive techniques for identifying liver fibrosis in post-LT settings found that VCTE was superior to acoustic radiation force impulse (ARFI) and serum biomarkers (e.g., AST/alanine transaminase [ALT] ratio, APRI, FibroTest [FT], and enhanced liver fibrosis test) [85].
Liver biopsy is the ultimate tool used to evaluate liver fibrosis. However, a liver biopsy is often complicated by its cumbersome nature, inadequate sampling, and extended sampling time. Often, the fibrosis distribution is heterogeneous and may evolve quickly, such as in BA [86]. Studies of HCV-infected adults showed that fibrosis scoring varied depending on sampling site in 33%–45% of patients [87,88].
Fibrosis scoring systems facilitate the standardization and comparison of biopsies. To date, studies in children have utilized different scoring systems developed for evaluating fibrosis in adults and specific etiologies. These include the METAVIR (developed for hepatitis C scoring in adults), Ishak, Batts and Ludwig, Brunt, and Knodell classifications. The METAVIR as the most commonly used according to our review of the literature (68% of studies comparing biopsy grades with noninvasive tools). Each scoring system relies on the progressive development of periportal fibrosis. However, fibrosis in children may assume other patterns, such as chicken wire fibrosis within lobules, perisinusoidal involvement, patchy fibrosis, and more rapid development as in BA [89,90]. Therefore, diagnostic efforts have concentrated on the identification and validation of noninvasive and accurate tools for evaluating fibrosis.
Various radiological methods and their respective advantages and disadvantages are depicted in Table 2.
VCTE is the most commonly used modality for evaluating liver stiffness worldwide, with FibroScan (Echosens, Paris, France) being the most common product [91]. VCTE requires its own probe and relies on creating 50-Hz frequency vibrations to induce shear waves. The velocity at which the generated shear waves travel is directly related to liver stiffness and increases in stiffer tissue [92].
VCTE is the most well-studied modality for estimating liver fibrosis in adult and pediatric settings. In 2018, Hwang et al. [93] performed a meta-analysis of 11 studies involving 723 patients to investigate the correlation between liver fibrosis biopsies and VCTE measurements. The AUROC for detecting stage ≥F2 fibrosis was 0.96, which remained stable across subgroup analyses involving patients aged ≥8 years and study design.
Despite the high accuracy and reproducibility of liver stiffness measurements (LSMs), limitations exist. Studies of healthy children found that LSMs were higher with increasing age and in boys [94,95]. In addition, LSM cutoffs vary by etiology. Studies of heterogeneous patient populations found a cutoff level of 7.5–13 kPa for detecting stage ≥ F3/F4 fibrosis [96-99]. In studies of infants with BA, before KPE, the cutoffs were 9.8–23.2 kPa [100-102]. Therefore, validation studies in large cohorts with subgroup analyses are needed to improve the reliability and accuracy of VCTE in clinical practice.
Similar to VCTE, 2-dimensional shear wave elastography (2D-SWE) and point shear wave elastography (p-SWE) use shear waves created by the liver parenchyma that travel with higher velocity in a stiffer medium. In contrast to VCTE, 2D-SWE and p-SWE use ARFI to induce shear waves. Both modalities employ a regular ultrasound probe to take measurements; however, 2D-SWE samples have a larger area than p-SWE samples [103].
A 2016 meta-analysis of 13 articles on 2D-SWE in the diagnosis of liver fibrosis in adults found high sensitivity and specificity of 2D-SWE across all stages of fibrosis [104]. In a meta-analysis of 12 studies of 2D-SWE accuracy in fibrosis in children, Kim et al. [105] computed a summary sensitivity, specificity, and AUROC of 81%, 91%, and 0.93 for detecting stage ≥ F2 fibrosis, respectively. Median cutoff values for detecting significant fibrosis as summarized by Jiang et al. [104] and Kim et al. [105] were 8.0 kPa and 9.4 kPa in adults and children, respectively.
Individual studies have evaluated the diagnostic performance of 2D-SWE in disease groups and patients with potential confounders. Dhyani et al. [106] and Galina et al. [107] compared the accuracy and cutoff values of 2D-SWE across hepatocellular and cholestatic disease groups. They both found higher LSM cutoff values for detecting fibrosis in cholestatic groups. Chen et al. [108] did not report a significant difference between LSM cutoffs in BA and non-BA cholestatic infants, supporting that cholestasis, but not BA alone, impacts LSM. Moreover, Tutar and Alhashmi et al. found that steatosis increases the LSM cutoff and reduces overall performance of 2D-SWE, while in their cohort of 68 patients with NAFLD Garcovich et al. reported AUROC values of 0.92 and 0.97 for detecting stage ≥F1 and ≥F2 fibrosis, respectively [109-111]. Dardanelli et al. [112] identified hemosiderosis as a confounder of 2D-SWE.
Overall, p-SWE has been described as a tool with greater reliability than transient elastography but lower accuracy than 2D-SWE [113]. In their 2016 systematic review, Andersen et al. [114] included 6 studies that evaluated p-SWE versus liver biopsy performance. They found poor distinctive ability for no, mild, and moderate fibrosis and evidence of confounding by necroinflammatory activity. Our search revealed 3 additional publications with AUROC values of 0.83–0.86 for detecting METAVIR scores ≥F3 with cutoffs. Across all studies, the cutoff for detecting F3 fibrosis was 2.0–2.17 m/sec [115-117].
Similar to US-based techniques, magnetic resonance elastography (MRE) involves the creation and measurement of shear wave velocity that travels through the liver parenchyma. Propagating shear waves were measured using standard MR phase-contrast imaging sequences with added motion encoding gradients [118]. Performance statistics in previous adult studies were very promising as they found AUROC values of 0.83–0.99 and 0.84–1.0 for detecting stage ≥F2 and ≥F3 fibrosis, respectively [119]. To date, 3 large studies have evaluated the role of MRE in staging liver fibrosis, with AUROC values of 0.53–0.93 [120-122]. All studies were relatively uniform in terms of the patient population (age 13–14.2 years) and disease (mainly hepatocellular pattern). However, the accuracy and reliability of MRE in NAFLD was conflicting between the Trout and Schwimmer et al. studies, with AUROC values of 0.53 and 0.93 for this population, respectively.
Table 3 provides a brief overview of the studies that evaluated composite scores in pediatric settings.
The APRI and FIB-4 scores were initially developed to monitor liver fibrosis progression in adults with hepatitis C [123,124]. Both are calculated using basic biochemistry, making them more accessible and cost-effective than radiological modalities.
The APRI was calculated using serum AST and platelet counts. The advancement of fibrosis reduces platelet counts in 2 ways: by reducing thrombopoietin generation by hepatocytes; and hypersplenism. Meanwhile, AST increases as chronic injury drives its release from mitochondria, and fibrosis diminishes clearance [125-127]. This pathophysiological derangement occurs later in the disease course, explaining why APRI has not always been a sensitive tool for detecting mild to moderate fibrosis [33,34]. Finally, APRI requires the use of the standard upper limit of normal for AST, which is 40 IU/L in most pediatric studies. Nevertheless, children often have lower baseline enzyme levels, which introduces potential bias to the score [128].
The FIB-4 index considers age-related differences in enzymes and ALT in addition to the components of APRI [123]. Despite these additional elements, APRI consistently outperformed FIB-4 in detecting fibrosis in both children and adults with liver disease [73,129-135]. One exception was the prediction of portal hypertension in a cohort of patients with CFLD, in which the FIB-4 index (AUROC, 0.91) had a superior AUROC to the APRI (AUROC, 0.71) [73].
FT is another composite score developed for the noninvasive evaluation of fibrosis in adults with chronic HCV. The FT combines age, sex, and 5 common serum markers: total bilirubin, a2-macroglobulin, haptoglobin, and gamma-glutamyl transferase [136]. Overall, the validation of FT in the pediatric cohort has been limited to relatively small studies comprising children with various CLD or viral hepatitis and did not reveal consistency [136-140].
Two indices were developed for noninvasive evaluation of liver fibrosis in children with NAFLD: Pediatric NAFLD Fibrosis Index (PNFI) and Pediatric NAFLD Fibrosis Score (PNFS). PNFI is based on age, waist circumference, and triglyceride levels. In a development cohort of 203 patients, the AUROC for predicting fibrosis was 0.85 [141]. Subsequently, Alkhouri et al. utilized PNFI in combination with an enhanced liver fibrosis test (ELF; including hyaluronic acid, procollagen-3, and tissue inhibitor of metalloproteinases-1) and VCTE. In both studies, ELF and VCTE were superior to PNFI, with AUROC values of 0.618–0.761 for detecting various fibrosis levels [142,143]. Similarly, Yang et al. [134] found that, across multiple diagnostic tests, PNFI had the lowest AUROC value in a cohort of 77 children with NAFLD. In 2014, Alkhouri et al. [131] developed PNFS in a cohort of 242 children with biopsy-proven NAFLD, which included ALT, alkaline phosphatase, platelet count, and gamma-glutamyl transferase levels. The AUROC value for this score was 0.74 for detecting stage ≥F3 fibrosis. However, external validation of this tool is still lacking [144].
Serum biomarkers for liver fibrosis have historically been classified as direct or indirect. Direct markers reflect ECM turnover, while indirect markers are proteins that are altered in the serum due to hepatic dysfunction [145]. Table 4 summarizes the most widely studied biomarkers in the pediatric population.
Fibrosis was initially considered irreversible with permanent tissue scarring. However, there is now compelling evidence of its resolution in the liver. Patients with liver fibrosis due to AIH, Wilson disease, and viral hepatitis show its regression after adequate treatment of the underlying disease process [146]. This phenomenon hints at the inherent physiology of fibrosis turnover. The cessation of ongoing injury is key to resolving fibrosis. Subsequently, the hepatic immune milieu tips suppress inflammation and recruit restorative macrophages that express MMPs, growth factors, and phagocytosis-related receptors for ECM clearance [147]. With the loss of activating signals, MFs are targeted for apoptosis via natural killer and γδ T cell-mediated pathways [148].
The resolution of fibrosis can interfere with ongoing injury. Unfortunately, despite progress in the molecular and genetic understanding of acquired and genetic liver disease in children, these conditions lack effective treatment except for a few such as viral hepatitis, autoimmune liver disease, and Wilson disease. Numerous trials investigating therapies directed at interfering with the disease process have incorporated liver fibrosis assessment as an endpoint. Several trials investigating the effect of metabolic modulation in NASH-NAFLD, such as through peroxisome proliferator-activated receptor-γ agonists (pioglitazone, rosiglitazone) on fibrosis regression, showed results ranging from decreased fibrosis to decreased fibrosis progression to no effect [149]. Similarly, ursodeoxycholic acid in primary biliary cirrhosis in a 4-year trial showed an overall improved rate of fibrosis progression, while a 2-year trial did not [149].
Translational research on antifibrotic therapy has focused on targeting fibrosis and fibrolysis pathways [150]. Among the inhibitors of HSC activation (e.g., blockers of cannabinoid receptor 1 angiotensin-converting enzyme, angiotensin receptor, endothelin 1 receptor), the farnesoid X receptor (FXR) antagonist, obeticholic acid (OCA), has shown the greatest promise. FXR is strongly expressed in the liver and intestines and acts as a master transcriptional regulator of several enterohepatic metabolic pathways [151]. In a recent multicenter phase III study of 931 patients with F2–F3 fibrosis due to NASH, placebo, 10-mg OCA, and 25-mg OCA groups showed 12%, 18%, and 71% improvement rates in fibrosis [152]. Another approach is to eliminate HSCs through mechanisms that drive apoptosis. Selonsertib is a novel apoptosis signal-regulating kinase 1 inhibitor that promotes apoptosis and downregulates HSC activation. A phase II trial comparing 6 mg and 18 mg of selonsertib in patients with NASH fibrosis reported that 30% versus 43% of patients had improved fibrosis on repeat biopsies, but these results were not reproduced in trials involving patients with F3–F4 fibrosis [153,154]. Intracellularly acting to interfere with collagen production, pirfenidone has also demonstrated promising results in patients with HCV [155]. In this phase II trial, 67% of patients had improved fibrosis scores at the end of the 24-month period. In addition to pharmacological interventions, cellular therapies are being actively explored. In a novel in vivo study, engineered T cells programmed against a cardiac fibroblast activation protein demonstrated a significant reduction in cardiac fibrosis in mice [156].
The epidemiology and burden of CLD in children remains unknown. According to transplant registries and the World Health Organization, more than 500 children undergo LT, while approximately 30% die while awaiting LT [157,158]. As most pediatric liver diseases have no definitive therapy, a better understanding of disease-specific fibrogenesis is mandatory for this vulnerable population. Irrespective of the cause, a panoply of signals drives HSC activation. Additionally, crosstalk between liver sinusoidal endothelial cells, hepatic fibroblasts, macrophages, injured hepatocytes, and other cell types contributes to these mechanisms. The exact role of each cell type should be clarified by single-cell transcriptomic and proteomic studies.
Despite substantial progress and significant investment in the development of noninvasive markers of liver fibrosis, most have not yet been validated in children. Thus, there is an urgent need to develop effective and reliable noninvasive scoring systems to replace biopsies in children. In terms of pathological evaluation, digital pathology methods that leverage machine learning and artificial intelligence must be validated to obtain more prognostic information from liver biopsies.
In conclusion, liver fibrosis is a complex dynamic process involving parenchymal and nonparenchymal liver cells as well as immune cells. Further studies exploring cell-cell interactions and etiology-specific elements of fibrogenesis and their link to disease, as well as the mechanism of fibrosis resolution, are crucial to the development of more effective therapeutic targets.
Fig. 1.
Cell-cell interactions and mediators driving hepatic stellate cell activation and fibrogenesis. Residing in the perisinusoidal space, HSCs become activated in response to a panoply of signals. LSECs, PFs, and HPCs also contribute to ECM deposition. Cytokines such as TGF-b, VEGF, PDGF, CTGF are implicated in promoting collagen production within an autocrine loop. Signals triggering this loop can be gut antigens acting on DAMP receptors on KCs, adipokines, products of cellular injury such as ROS, and some innate and adaptive immune cells. On the other hand, some immune cells participate in inhibition and removal of fibrosis. NK cells resident in the liver are antifibrotic through apoptosis of HSCs. Th1, Treg, and CD8 memory T cells also participate in fibrosis resolution. HSC, hepatic stellate cell; qHSC, quiescent HSC; aHSC, activated HSC; LSEC, liver sinusoidal endothelial cell; PF, portal fibroblast; HPC, hepatic progenitor cell; ECM, excess extracellular matrix; TGF-β, transforming growth factor-β; VEGF, vascular endothelial growth factor; PDGF, platelet-derived growth factor; CTGF, connective TGF; DAMP, damage-associated molecular pattern; KC, Kupffer cell; ROS, reactive oxygen species; NK, natural killer; Th1, T helper 1; Treg, regulatory T; TLR, toll-like receptor; LPS, lipopolysaccharide; ER, endoplasmic reticulum.
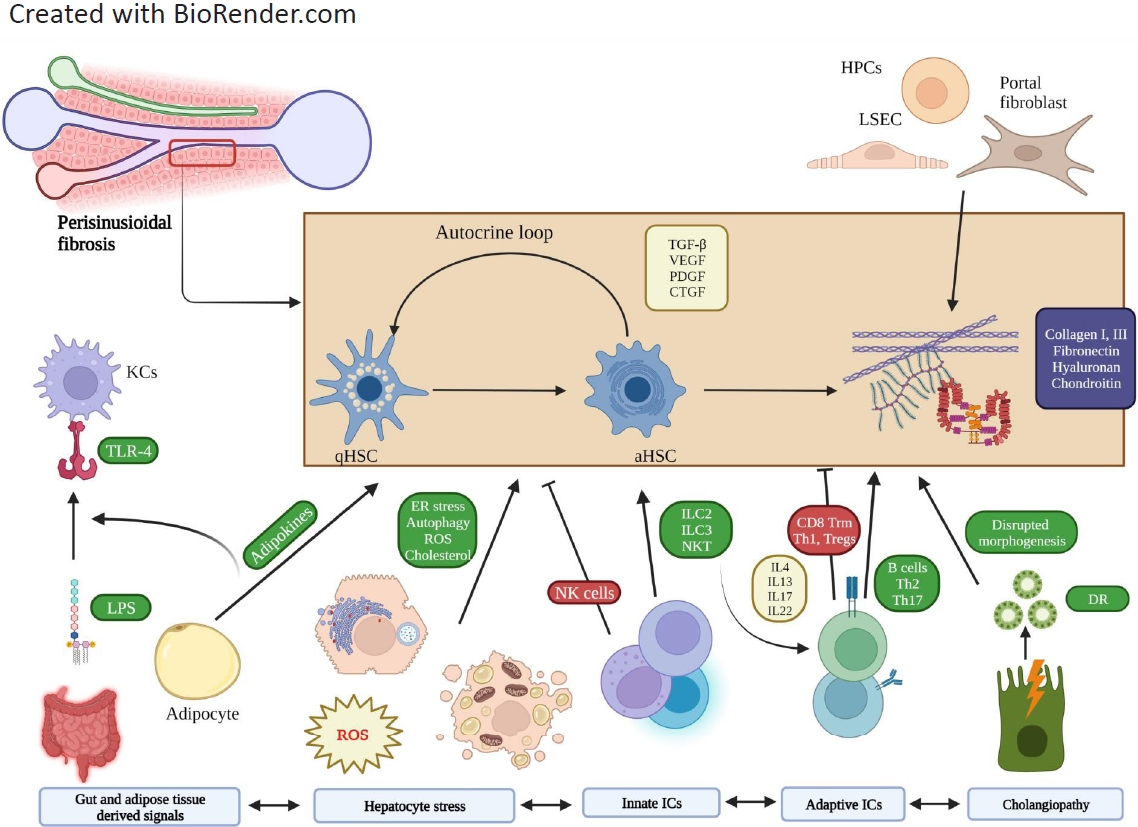
Fig. 2.
Distinct features of pediatric physiology that may contribute to the unique fibrosis pattern and progression seen in children. The process of neonatal or pediatric liver fibrosis differs from that in adults. Neonatal liver clearly lacks the mature architecture and enzyme levels. Similarly, cholangiocytes have immature barrier mechanisms that protect them from bile flow. Interestingly, the neonatal liver has a robust fibrogenic environment despite higher regenerative potential of the skin. The neonatal immune system is immature. CD8 T cells tend to differentiate into effector cells, while the hepatic immune system significantly differs in functionality and composition. The pediatric microbiome shifts across ages and impacts many disorders. CYP450, cytochromes P450; α-SMA, α-smooth muscle actin; Th, T helper; KC, Kupffer cell.

Table 1.
Frequency and characteristics of fibrosis development in chronic pediatric liver diseases
| Disease | Age of presentation | Age of fibrosis development | Risk of cirrhosis | Biopsy findings |
|---|---|---|---|---|
| Congenital hepatic fibrosis [159] | Infancy, childhood | Childhood, adolescence | High (by 5-13 years) | Triads (bile duct abnormality, portal vein hypoplasia, diffuse periportal fibrosis/white bands encircling hepatic lobules) |
| Cystic fibrosis liver disease [160] | Variable | Childhood, early adulthood | High (10% by 30 years old) | Biliary obstruction and periportal fibrosis |
| Chronic hepatitis B [161] | May be asymptomatic through childhood (immune tolerant stage) | 89.8% by median of 3 years of age | 1-5% of HbE+children | Periportal fibrosis |
| Chronic hepatitis C | Asymptomatic through childhood, 10% hepatomegaly | 50% with fibrosis at initial biopsy (7.4 years), slowly progressive | Low, 1.7%-1.8% in 2 studies | Mild periportal fibrosis, less commonly peri-sinusoidal fibrosis |
| Biliary atresia [162] | Neonatal | Neonatal | High | Biliary sclerosis and obliteration, loose periportal fibrosis |
| Primary sclerosing cholangitis [13] | Childhood, adolescence | 41% with METAVIR F3-4 fibrosis at initial biopsy (age 14.0 years) | High, 38% after 10 years in 1 study | Periductal fibrosis of extrahepatic ducts, periportal fibrosis |
| NAFLD/NASH [49] | Age 10-13 years, elevated ALT | 82% with fibrosis at initial biopsy (age 13.0 years) | 10%-25% have progression | Steatosis, ballooning, infiltration of inflammatory cells, pericellular chicken wire fibrosis |
| Fontan-associated Ld [163] | Silent, 10 years after Fontan | Adolescence | 33%-68% | Centrilobular hepatocyte atrophy, sinusoidal fibrosis |
| Alagille syndrome [164] | Early infancy | Slower than BA; by 20 years of age, 40% developed PH | 10%-50% | Bile duct proliferation (early), bile duct paucity (late), lymphocyte infiltration of biliary epithelium, peribiliary fibrosis |
| PFIC 1-2 [165] | Early infancy | First years of life | High | Cholestasis, centrilobular and portal fibrosis, no true ductular proliferation (fibrosis more prominent in type II) |
| PFIC 3 [165] | Up to young adulthood | Mean age of 7.5 | High | Cholestasis, portal fibrosis, has true ductular proliferation |
| Autoimmune hepatitis [166] | Puberty (type I), early childhood (type II) | Cirrhosis in 55% at diagnosis | High, 30%-55% at presentation but regression at advanced fibrosis stage common | Interface hepatitis; portal/periportal, portalportal, portal-central fibrosis |
Table 2.
Radiological assessment tools for liver fibrosis
| Modality | Mechanism | Advantage | Disadvantage |
|---|---|---|---|
| Vibration-controlled transient elastography | Vibration induced shear waves |
Quick bedside assessment Pediatric probe available Studied across wide range of liver diseases in children and adults |
No real-time USG guidance Poor performance in congestion, obesity, inflammation [167,168] |
| 2-Dimensional-shear wave elastography | Acoustic radiation force impulse creates shear waves |
Implemented in US scanner Visualization of liver parenchyma Less limited by movement Measures multiple levels simultaneously with color-coding of stiffness values |
May be affected by steatosis/inflammation [111] Age dependent increase [169] Cutoff values vendor/technique-specific [170] Effect of body mass index unclear [111,171] |
| Point shear wave elasto-graphy | Acoustic radiation force impulse creates shear waves |
Implemented in US scanner Visualization of liver parenchyma |
Measures one region of interest May be affected by steatosis/inflammation [111] Cutoff values vendor/technique-specific [116] |
| Magnetic resonance (MR) elastography | Acoustic waves delivered by driver placed on patient |
MR scanner is the probe Additional cross-sectional imaging Not limited by anatomic factors |
Higher cost Longer duration May be affected by steatosis [120] Breath-holding necessary |
Table 3.
Composite fibrosis scores evaluated in children with liver diseases (see
Supplementary Table for details)
AUC, area under the curve; CLD, chronic liver disease; BA, biliary atresia; NAFLD, nonalcoholic liver disease; IFALD, intestinal failure-associated liver disease; APRI, aspartate aminotransferase to platelet ratio index; CFLD, cystic fibrosis-related liver disease; AGS, Alagille syndrome; PSC, primary sclerosing cholangitis; PFIC, progressive familial intrahepatic cholestasis; FIB-4, fibrosis-4.
Table 4.
Most studied serum biomarkers of fibrosis in pediatric hepatology
| Biomarker | Structure/function | Expected change in fibrosis | Conditions evaluated | AUC value |
|---|---|---|---|---|
| Hyaluronic acid | Glycosaminoglycan Cleared by hepatocytes by diffusing through sinusoidal endothelium | Increased in fibrosis due to thickening of sinusoidal endothelium May be increased after foods or drinks [172] | NAFLD, viral hepatitis, CFLD | 0.67–0.88 [71,96,97,108,129,173-176] |
| Type IV collagen | Crucial component of hepatic basement membrane [177,178] | Increases with grade of fibrosis due to turnover [179] | Viral hepatitis, CFLD, BA | 0.79 for detecting ≥F3 in BA, not significant for rest [71,108,129,197] |
| Procollagen III aminopeptide | Type III collagen undergoes N-terminal cleavage at procollagen stage of synthesis [177] | Increases due to turnover May be elevated in chronic inflammatory states [180,181] | BA, non-BA infantile cholestasis, NAFLD |
0.843, 0.92 No correlation in one study [108,135,182] |
| Laminin | Noncollagenous glycoprotein found in hepatic BM | Increases due to deposition around perisinusoidal space [183] | Non-BA infantile cholestasis, viral hepatitis, NAFLD | 0.84 for viral hepatitis, no correlation in others [108,173,174] |
| YKL-40 | Inflammatory glycoprotein secreted from macrophages [184] | Increases due to macrophage activation Increased in many conditions [185] | Viral hepatitis, NAFLD | 0.387, 0.52 [96,173,186] |
| Monocyte chemoattractant protein 1 |
Primary ligand for chemokine receptor C-C chemokine receptor 2, attracts monocytes Role in HSC activation via Sphingosine kinase 1 [187-190] |
Increased in liver inflammation/fibrosis [190,191] | Viral hepatitis | 0.813 [129] |
| Soluble Fas | Triggers apoptosis in hepatocytes | Increased in severe fibrosis in adult studies, detected to be lower in 1 pediatric study [129] | Viral hepatitis | 0.719—0.82 [129] |
| Cytokeratin-18 fragments | Major intermediate filament in hepatocytes | Increases as a marker of hepatocyte apop-tosiscleaved by caspases) [192] | NAFLD | 0.66–0.842 [97,173,193] |
| Autotaxin |
Glycoprotein enzyme Catalyzes hydrolysis of LPC to LPA stimulated HSCs in a murine model; degraded by liver sinusoidal endothelium [194] |
Overexpressed in BA liver [195] Increased due to impaired degradation [196] |
BA | 0.93 [197] |
| Mac-2 binding protein glycosylation isomer | Secreted from HSCs and activates KCs [198] |
Increases as a biomarker of HSC activation May predict activation of viral hepatitis, carcinogenesis, and liver failure [199] |
BA | 0.90—0.95[197,200] |
References
1. Kelly DA. Paediatric liver disease: lessons for adult practice. Lancet Gastroenterol Hepatol 2017;2:390–2.


2. Arya G, Balistreri WF. Pediatric liver disease in the United States: epidemiology and impact. J Gastroenterol Hepatol 2002;17:521–5.


3. Organ Procurement and Transplantation Network. National data [Internet]. Richmond (VA): Organ Procurement and Transplantation Network; 2022 [cited 2022 Sep 10]. Available from: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/.
4. Albanis E, Friedman SL. HEPATIC FIBROSIS: pathogenesis and principles of therapy. Clin Liver Dis 2001;5:315. –34. v-vi.

5. George M, Paci P, Taner T. Significance of progressive liver fibrosis in pediatric liver transplants: a review of current evidence. World J Gastroenterol 2020;26:1987–92.



7. Wake K. "Sternzellen" in the liver: perisinusoidal cells with special reference to storage of vitamin A. Am J Anat 1971;132:429–62.


8. Mederacke I, Hsu CC, Troeger JS, Huebener P, Mu X, Dapito DH, et al. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nature Commun 2013;4:2823.




9. Serinet MO, Wildhaber BE, Broué P, Lachaux A, Sarles J, Jacquemin E, et al. Impact of age at Kasai operation on its results in late childhood and adolescence: a rational basis for biliary atresia screening. Pediatrics 2009;123:1280–6.



10. Chardot C, Buet C, Serinet MO, Golmard JL, Lachaux A, Roquelaure B, et al. Improving outcomes of biliary atresia: French national series 1986-2009. J Hepatol 2013;58:1209–17.


11. Deneau M, Jensen MK, Holmen J, Williams MS, Book LS, Guthery SL. Primary sclerosing cholangitis, autoimmune hepatitis, and overlap in Utah children: epidemiology and natural history. Hepatology 2013;58:1392–400.


12. Fagundes EDT, Ferreira AR, Hosken CC, Queiroz TCN. Primary sclerosing cholangitis in children and adolescents. Arq Gastroenterol 2017;54:286–91.


13. Miloh T, Arnon R, Shneider B, Suchy F, Kerkar N. A retrospective single-center review of primary sclerosing cholangitis in children. Clin Gastroenterol Hepatol 2009;7:239–45.


14. Valentino PL, Wiggins S, Harney S, Raza R, Lee CK, Jonas MM. The natural history of primary sclerosing cholangitis in children: a large singlecenter longitudinal cohort study. J Pediatr Gastroenterol Nutr 2016;63:603–9.


15. Wiecek S, Wojtyniak A, Pindur B, Machnikowska-Sokołowska M, Gruszczyńska K, Grzybowska-Chlebowczyk U. Analysis of the clinical course of primary sclerosing cholangitis in paediatric population-single center study. Medicina (Kaunas) 2021;57:663.



16. Yoon J, Oh SH, Kim HJ, Park SH, Ye BD, Yang SK, et al. Primary sclerosing cholangitis with inflammatory bowel disease in Korean children. Pediatr Gastroenterol Hepatol Nutr 2015;18:268–75.



17. Cotter JM, Browne LP, Capocelli KE, McCoy A, Mack CL. Lack of correlation of liver tests with fibrosis stage at diagnosis in pediatric primary sclerosing cholangitis. J Pediatr Gastroenterol Nutr 2018;66:227–33.


18. Batres LA, Russo P, Mathews M, Piccoli DA, Chuang E, Ruchelli E. Primary sclerosing cholangitis in children: a histologic follow-up study. Pediatr Dev Pathol 2005;8:568–76.



19. Sørensen J, Nielsen OH, Andersson M, Ainsworth MA, Ytting H, Bélard E, et al. Inflammatory bowel disease with primary sclerosing cholangitis: a Danish population-based cohort study 1977-2011. Liver Int 2018;38:532–41.



20. Deneau MR, Mack C, Mogul D, Perito ER, Valentino PL, Amir AZ, et al. Oral vancomycin, ursodeoxycholic acid, or no therapy for pediatric primary sclerosing cholangitis: a matched analysis. Hepatology 2021;73:1061–73.




21. Laborda TJ, Jensen MK, Kavan M, Deneau M. Treatment of primary sclerosing cholangitis in children. World J Hepatol 2019;11:19–36.



22. Haisma SM, Weersma RK, Joosse ME, de Koning BAE, de Meij T, Koot BGP, et al. Exome sequencing in patient-parent trios suggests new candidate genes for early-onset primary sclerosing cholangitis. Liver Int 2021;41:1044–57.




23. Karlsen TH, Franke A, Melum E, Kaser A, Hov JR, Balschun T, et al. Genome-wide association analysis in primary sclerosing cholangitis. Gastroenterology 2010;138:1102–11.


24. Liu JZ, Hov JR, Folseraas T, Ellinghaus E, Rushbrook SM, Doncheva NT, et al. Dense genotyping of immune-related disease regions identifies nine new risk loci for primary sclerosing cholangitis. Nat Genet 2013;45:670–5.




25. Kohut TJ, Gilbert MA, Loomes KM. Alagille syndrome: a focused review on clinical features, genetics, and treatment. Semin Liver Dis 2021;41:525–37.


26. Kamath BM, Yin W, Miller H, Anand R, Rand EB, Alonso E, et al. Outcomes of liver transplantation for patients with Alagille syndrome: the studies of pediatric liver transplantation experience. Liver Transpl 2012;18:940–8.


27. Lykavieris P, Hadchouel M, Chardot C, Bernard O. Outcome of liver disease in children with Alagille syndrome: a study of 163 patients. Gut 2001;49:431–5.



28. Vandriel S, Wang JS, Li L, Piccoli DA, Loomes KM, Sokal E, et al. Clinical features and outcomes in an international cohort of 731 Alagille syndrome patients from 19 countries. The Liver Meeting AASLD (American Association of the Study of Liver Diseases); 2019;Nov;8. –12. Boston (MA), USA. In: Hepatology 2019. http://hdl.handle.net/2078.1/222803.
29. Fabris L, Cadamuro M, Guido M, Spirli C, Fiorotto R, Colledan M, et al. Analysis of liver repair mechanisms in Alagille syndrome and biliary atresia reveals a role for notch signaling. Am J Pathol 2007;171:641–53.



30. Fiorotto R, Raizner A, Morell CM, Torsello B, Scirpo R, Fabris L, et al. Notch signaling regulates tubular morphogenesis during repair from biliary damage in mice. J Hepatol 2013;59:124–30.



32. MacLachlan JH, Cowie BC. Hepatitis B virus epidemiology. Cold Spring Harb Perspect Med 2015;5:a021410.



33. Goodman ZD, Makhlouf HR, Liu L, Balistreri W, Gonzalez-Peralta RP, Haber B, et al. Pathology of chronic hepatitis C in children: liver biopsy findings in the Peds-C Trial. Hepatology 2008;47:836–43.



34. Bortolotti F, Verucchi G, Cammà C, Cabibbo G, Zancan L, Indolfi G, et al. Long-term course of chronic hepatitis C in children: from viral clearance to end-stage liver disease. Gastroenterology 2008;134:1900–7.


35. Bortolotti F, Calzia R, Cadrobbi P, Giacchini R, Ciravegna B, Armigliato M, et al. Liver cirrhosis associated with chronic hepatitis B virus infection in childhood. J Pediatr 1986;108:224–7.


36. Rodriguez-Baez N, Murray KF, Kleiner DE, Ling SC, Rosenthal P, Carlin K, et al. Hepatic histology in treatment-naïve children with chronic hepatitis B infection living in the United States and Canada. J Pediatr Gastroenterol Nutr 2020;71:99–105.



37. Łotowska JM, Lebensztejn DM. Immunoreactive hepatic stellate cells in biopsy material in children with chronic hepatitis B. The first report in pediatric patients. Pol J Pathol 2015;66:224–30.

38. Lotowska JM, Sobaniec-Lotowska ME, Lebensztejn DM. Ultrastructural characteristics of the respective forms of hepatic stellate cells in chronic hepatitis B as an example of high fibroblastic cell plasticity. The first assessment in children. Adv Med Sci 2018;63:127–33.


39. Lotowska JM, Sobaniec-Lotowska ME, Lebensztejn DM. Electron microscopic alterations in intermediate hepatocyte-like cells in children with chronic hepatitis B: the first report in pediatric patients. Eur J Gastroenterol Hepatol 2010;22:741–7.


40. Sobaniec-Lotowska ME, Lotowska JM, Lebensztejn DM. Ultrastructure of oval cells in children with chronic hepatitis B, with special emphasis on the stage of liver fibrosis: the first pediatric study. World J Gastroenterol 2007;13:2918–22.



41. Strader DB, Wright T, Thomas DL, Seeff LB. Diagnosis, management, and treatment of hepatitis C. Hepatology 2004;39:1147–71.


42. Gregorio GV, Portmann B, Reid F, Donaldson PT, Doherty DG, McCartney M, et al. Autoimmune hepatitis in childhood: a 20-year experience. Hepatology 1997;25:541–7.


43. Mieli-Vergani G, Heller S, Jara P, Vergani D, Chang MH, Fujisawa T, et al. Autoimmune hepatitis. J Pediatr Gastroenterol Nutr 2009;49:158–64.


44. Maia JM, Maranhão Hde S, Sena LV, Rocha LR, Medeiros IA, Ramos AM. Hepatic stellate cell activation and hepatic fibrosis in children with type 1 autoimmune hepatitis: an immunohistochemical study of paired liver biopsies before treatment and after clinical remission. Eur J Gastroenterol Hepatol 2010;22:264–9.


45. Abdalla AF, Zalata KR, Ismail AF, Shiha G, Attiya M, Abo-Alyazeed A. Regression of fibrosis in paediatric autoimmune hepatitis: morphometric assessment of fibrosis versus semiquantiatative methods. Fibrogenesis Tissue Repair 2009;2:2.




46. Salem M, Ehsan N, El-Behairy B, Hussein M, Salama E. Regression of liver fibrosis in children with autoimmune hepatitis who responded to immunosuppressant treatment. Arch Dis Child 2008;93(Suppl 2): pw572.
47. Aggarwal A, Puri K, Thangada S, Zein N, Alkhouri N. Nonalcoholic fatty liver disease in children: recent practice guidelines, where do they take us? Curr Pediatr Rev 2014;10:151–61.


48. Atsawarungruangkit A, Elfanagely Y, Pan J, Anderson K, Scharfen J, Promrat K. Prevalence and risk factors of steatosis and advanced fibrosis using transient elastography in the United States' adolescent population. World J Hepatol 2021;13:790–803.



49. Schwimmer JB, Behling C, Newbury R, Deutsch R, Nievergelt C, Schork NJ, et al. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology 2005;42:641–9.


50. Kim MJ, Lee KJ. Analysis of the dietary factors associated with suspected pediatric nonalcoholic fatty liver disease and potential liver fibrosis: Korean National Health and Nutrition Examination Survey 2014-2017. BMC Pediatr 2020;20:121.




51. Ting YW, Wong SW, Anuar Zaini A, Mohamed R, Jalaludin MY. Metabolic syndrome is associated with advanced liver fibrosis among pediatric patients with non-alcoholic fatty liver disease. Front Pediatr 2019;7:491.



52. Moran-Lev H, Cohen S, Webb M, Yerushalmy-Feler A, Amir A, Gal DL, et al. Higher BMI predicts liver fibrosis among obese children and adolescents with NAFLD - an interventional pilot study. BMC Pediatrics 2021;21:385.




53. Xu R, Tao A, Zhang S, Deng Y, Chen G. Association between patatin-like phospholipase domain containing 3 gene (PNPLA3) polymorphisms and nonalcoholic fatty liver disease: a HuGE review and meta-analysis. Sci Rep 2015;5:9284.




54. Carpino G, Pastori D, Baratta F, Overi D, Labbadia G, Polimeni L, et al. PNPLA3 variant and portal/periportal histological pattern in patients with biopsy-proven non-alcoholic fatty liver disease: a possible role for oxidative stress. Sci Rep 2017;7:15756.




55. Friedman JE, Dobrinskikh E, Alfonso-Garcia A, Fast A, Janssen RC, Soderborg TK, et al. Pyrroloquinoline quinone prevents developmental programming of microbial dysbiosis and macrophage polarization to attenuate liver fibrosis in offspring of obese mice. Hepatol Commun 2018;2:313–28.




56. Khalaf RT, Sokol RJ. New insights into intestinal failure-associated liver disease in children. Hepatology 2020;71:1486–98.




57. Lauriti G, Zani A, Aufieri R, Cananzi M, Chiesa PL, Eaton S, et al. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: a systematic review. JPEN J Parenter Enteral Nutr 2014;38:70–85.



58. Fitzgibbons SC, Jones BA, Hull MA, Zurakowski D, Duro D, Duggan C, et al. Relationship between biopsy-proven parenteralnutrition-associated liver fibrosis and biochemical cholestasis in children with short bowel syndrome. J Pediatr Surg 2010;45:95. –9. discussion 9.



59. Mutanen A, Lohi J, Heikkilä P, Koivusalo AI, Rintala RJ, Pakarinen MP. Persistent abnormal liver fibrosis after weaning off parenteral nutrition in pediatric intestinal failure. Hepatology 2013;58:729–38.


60. El Kasmi KC, Anderson AL, Devereaux MW, Vue PM, Zhang W, Setchell KD, et al. Phytosterols promote liver injury and Kupffer cell activation in parenteral nutrition-associated liver disease. Sci Transl Med 2013;5:206ra137.



61. Mutanen A, Lohi J, Heikkilä P, Jalanko H, Pakarinen MP. Liver inflammation relates to decreased canalicular bile transporter expression in pediatric onset intestinal failure. Ann Surg 2018;268:332–9.


62. Mutanen A, Lohi J, Sorsa T, Jalanko H, Pakarinen MP. Features of liver tissue remodeling in intestinal failure during and after weaning off parenteral nutrition. Surgery 2016;160:632–42.


63. Ward CJ, Hogan MC, Rossetti S, Walker D, Sneddon T, Wang X, et al. The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptor-like protein. Nat Genet 2002;30:259–69.



64. Desmet VJ. Congenital diseases of intrahepatic bile ducts: variations on the theme “ductal plate malformation”. Hepatology 1992;16:1069–83.


65. Zhu B, Du Z, Wang Z, Li Y, Zhang J, Zhu H. Congenital hepatic fibrosis in children and adults: clinical manifestations, management, and outcome-case series and literature review. Gastroenterol Res Pract 2020;2020:8284274.




66. Gunay-Aygun M, Font-Montgomery E, Lukose L, Gerstein MT, PiwnicaWorms K, Choyke P, et al. Characteristics of congenital hepatic fibrosis in a large cohort of patients with autosomal recessive polycystic kidney disease. Gastroenterology 2013;144:112. –21. e2.



67. Arikan C, Ozgenc F, Akman SA, Kilic M, Tokat Y, Yagci RV, et al. Impact of liver transplantation on renal function of patients with congenital hepatic fibrosis associated with autosomal recessive polycystic kidney disease. Pediatr Transplant 2004;8:558–60.


68. Irie R, Nakazawa A, Sakamoto S, Takeda M, Yanagi Y, Shimizu S, et al. Living donor liver transplantation for congenital hepatic fibrosis in children. Pathol Int 2020;70:348–54.



69. Boëlle PY, Debray D, Guillot L, Clement A, Corvol H. Cystic fibrosis liver disease: outcomes and risk factors in a large cohort of french patients. Hepatology 2019;69:1648–56.




70. Lewindon PJ, Shepherd RW, Walsh MJ, Greer RM, Williamson R, Pereira TN, et al. Importance of hepatic fibrosis in cystic fibrosis and the predictive value of liver biopsy. Hepatology 2011;53:193–201.


71. Pereira TN, Lewindon PJ, Smith JL, Murphy TL, Lincoln DJ, Shepherd RW, et al. Serum markers of hepatic fibrogenesis in cystic fibrosis liver disease. J Hepatol 2004;41:576–83.


72. Lewindon PJ, Puertolas-Lopez MV, Ramm LE, Noble C, Pereira TN, Wixey JA, et al. Accuracy of transient elastography data combined with APRI in detection and staging of liver disease in pediatric patients with cystic fibrosis. Clin Gastroenterol Hepatol 2019;17:2561. –9. e5.


73. Leung DH, Khan M, Minard CG, Guffey D, Ramm LE, Clouston AD, et al. Aspartate aminotransferase to platelet ratio and fibrosis-4 as biomarkers in biopsy-validated pediatric cystic fibrosis liver disease. Hepatology 2015;62:1576–83.


75. Emamaullee J, Zaidi AN, Schiano T, Kahn J, Valentino PL, Hofer RE, et al. Fontan-associated liver disease. Circulation 2020;142:591–604.



76. Martinelli J, Habes D, Majed L, Guettier C, Gonzalès E, Linglart A, et al. Long-term outcome of liver transplantation in childhood: a study of 20- year survivors. Am J Transplant 2018;18:1680–9.



77. Ekong UD, Melin-Aldana H, Seshadri R, Lokar J, Harris D, Whitington PF, et al. Graft histology characteristics in long-term survivors of pediatric liver transplantation. Liver Transpl 2008;14:1582–7.


78. Evans HM, Kelly DA, McKiernan PJ, Hübscher S. Progressive histological damage in liver allografts following pediatric liver transplantation. Hepatology 2006;43:1109–17.


79. Fouquet V, Alves A, Branchereau S, Grabar S, Debray D, Jacquemin E, et al. Long-term outcome of pediatric liver transplantation for biliary atresia: a 10-year follow-up in a single center. Liver Transpl 2005;11:152–60.


80. Sanada Y, Matsumoto K, Urahashi T, Ihara Y, Wakiya T, Okada N, et al. Protocol liver biopsy is the only examination that can detect mid-term graft fibrosis after pediatric liver transplantation. World J Gastroenterol 2014;20:6638–50.



81. Scheenstra R, Peeters PM, Verkade HJ, Gouw AS. Graft fibrosis after pediatric liver transplantation: ten years of follow-up. Hepatology 2009;49:880–6.


82. Qin T, Fu J, Verkade HJ. The role of the gut microbiome in graft fibrosis after pediatric liver transplantation. Hum Genet 2021;140:709–24.




83. Varma S, Ambroise J, Komuta M, Latinne D, Baldin P, Reding R, et al. Progressive fibrosis is driven by genetic predisposition, allo-immunity, and inflammation in pediatric liver transplant recipients. EBioMedicine 2016;9:346–55.



84. Briem-Richter A, Ganschow R, Sornsakrin M, Brinkert F, Schirmer J, Schaefer H, et al. Liver allograft pathology in healthy pediatric liver transplant recipients. Pediatr Transplant 2013;17:543–9.


85. Vo HD, Harp KA, Mauch TJ. Diagnostic performance of non-invasive tests for evaluation of hepatic graft fibrosis in pediatric liver transplantation: a scoping review. Transplant Rev (Orlando) 2020;34:100568.


86. Azar G, Beneck D, Lane B, Markowitz J, Daum F, Kahn E. Atypical morphologic presentation of biliary atresia and value of serial liver biopsies. J Pediatr Gastroenterol Nutr 2002;34:212–5.


87. Siddique I, El-Naga HA, Madda JP, Memon A, Hasan F. Sampling variability on percutaneous liver biopsy in patients with chronic hepatitis C virus infection. Scand J Gastroenterol 2003;38:427–32.


88. Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 2002;97:2614–8.


89. Leung DH. Hepatic fibrosis scores and serum biomarkers in pediatric hepatology. Clin Liver Dis (Hoboken) 2017;9:125–30.




90. Alisi A, de Vito R, Monti L, Nobili V. Liver fibrosis in paediatric liver diseases. Best Pract Res Clin Gastroenterol 2011;25:259–68.


91. Tapper EB, Castera L, Afdhal NH. FibroScan (vibration-controlled transient elastography): where does it stand in the United States practice. Clin Gastroenterol Hepatol 2015;13:27–36.


92. Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol 2008;48:835–47.


93. Hwang JY, Yoon HM, Kim JR, Lee JS, Jung AY, Kim KM, et al. Diagnostic performance of transient elastography for liver fibrosis in children: a systematic review and meta-analysis. AJR Am J Roentgenol 2018;211:W257–66.


94. Jain V, Poddar U, Negi TS, Saraswat VA, Krishnani N, Yachha SK, et al. Utility and accuracy of transient elastography in determining liver fibrosis: a case-control study. Eur J Pediatr 2020;179:671–7.



95. Mjelle AB, Mulabecirovic A, Havre RF, Rosendahl K, Juliusson PB, Olafsdottir E, et al. Normal liver stiffness values in children: a comparison of three different elastography methods. J Pediatr Gastroenterol Nutr 2019;68:706–12.



96. Lee CK, Perez-Atayde AR, Mitchell PD, Raza R, Afdhal NH, Jonas MM. Serum biomarkers and transient elastography as predictors of advanced liver fibrosis in a United States cohort: the Boston children's hospital experience. J Pediatr 2013;163:1058. –64. e2.


97. Fitzpatrick E, Quaglia A, Vimalesvaran S, Basso MS, Dhawan A. Transient elastography is a useful noninvasive tool for the evaluation of fibrosis in paediatric chronic liver disease. J Pediatr Gastroenterol Nutr 2013;56:72–6.


98. Teufel-Schäfer U, Flechtenmacher C, Fichtner A, Hoffmann GF, Schenk JP, Engelmann G. Transient elastography correlated to four different histological fibrosis scores in children with liver disease. Eur J Pediatr 2021;180:2237–44.




99. Behairy Bel S, Sira MM, Zalata KR, Salama el SE, Abd-Allah MA. Transient elastography compared to liver biopsy and morphometry for predicting fibrosis in pediatric chronic liver disease: Does etiology matter? World J Gastroenterol 2016;22:4238–49.



100. Hukkinen M, Lohi J, Heikkilä P, Kivisaari R, Jahnukainen T, Jalanko H, et al. Noninvasive evaluation of liver fibrosis and portal hypertension after successful portoenterostomy for biliary atresia. Hepatol Commun 2019;3:382–91.




101. Shin NY, Kim MJ, Lee MJ, Han SJ, Koh H, Namgung R, et al. Transient elastography and sonography for prediction of liver fibrosis in infants with biliary atresia. J Ultrasound Med 2014;33:853–64.



102. Shen QL, Chen YJ, Wang ZM, Zhang TC, Pang WB, Shu J, et al. Assessment of liver fibrosis by Fibroscan as compared to liver biopsy in biliary atresia. World J Gastroenterol 2015;21:6931–6.



103. Ozturk A, Grajo JR, Dhyani M, Anthony BW, Samir AE. Principles of ultrasound elastography. Abdom Radiol (NY) 2018;43:773–85.




104. Jiang T, Tian G, Zhao Q, Kong D, Cheng C, Zhong L, et al. Diagnostic accuracy of 2D-shear wave elastography for liver fibrosis severity: a metaanalysis. PLoS One 2016;11:e0157219.



105. Kim JR, Suh CH, Yoon HM, Lee JS, Cho YA, Jung AY. The diagnostic performance of shear-wave elastography for liver fibrosis in children and adolescents: a systematic review and diagnostic meta-analysis. Eur Radiol 2018;28:1175–86.



106. Dhyani M, Gee MS, Misdraji J, Israel EJ, Shah U, Samir AE. Feasibility study for assessing liver fibrosis in paediatric and adolescent patients using real-time shear wave elastography. J Med Imaging Radiat Oncol 2015;59:687. –94. quiz 751.



107. Galina P, Alexopoulou E, Mentessidou A, Mirilas P, Zellos A, Lykopoulou L, et al. Diagnostic accuracy of two-dimensional shear wave elastography in detecting hepatic fibrosis in children with autoimmune hepatitis, biliary atresia and other chronic liver diseases. Pediatr Radiol 2021;51:1358–68.



108. Chen H, Zhou L, Liao B, Cao Q, Jiang H, Zhou W, et al. Twodimensional shear wave elastography predicts liver fibrosis in jaundiced infants with suspected biliary atresia: a prospective study. Korean J Radiol 2021;22:959–69.




109. Garcovich M, Veraldi S, Di Stasio E, Zocco MA, Monti L, Tomà P, et al. Liver stiffness in pediatric patients with fatty liver disease: diagnostic accuracy and reproducibility of shear-wave elastography. Radiology 2017;283:820–7.


110. Tutar O, Beşer ÖF, Adaletli I, Tunc N, Gulcu D, Kantarci F, et al. Shear wave elastography in the evaluation of liver fibrosis in children. J Pediatr Gastroenterol Nutr 2014;58:750–5.


111. Alhashmi GH, Gupta A, Trout AT, Dillman JR. Two-dimensional ultrasound shear wave elastography for identifying and staging liver fibrosis in pediatric patients with known or suspected liver disease: a clinical effectiveness study. Pediatr Radiol 2020;50:1255–62.



112. Dardanelli EP, Orozco ME, Lostra J, Laprida C, Lulkin S, Bosaleh AP, et al. Bidimensional shear-wave elastography for assessing liver fibrosis in children: a proposal of reference values that correlate with the histopathological Knodell-Ishak score. Pediatr Radiol 2020;50:817–26.



114. Andersen SB, Ewertsen C, Carlsen JF, Henriksen BM, Nielsen MB. Ultrasound elastography is useful for evaluation of liver fibrosis in children-a systematic review. J Pediatr Gastroenterol Nutr 2016;63:389–99.


115. Hanquinet S, Rougemont AL, Courvoisier D, Rubbia-Brandt L, McLin V, Tempia M, et al. Acoustic radiation force impulse (ARFI) elastography for the noninvasive diagnosis of liver fibrosis in children. Pediatr Radiol 2013;43:545–51.



116. Özkan MB, Bilgici MC, Eren E, Caltepe G, Yilmaz G, Kara C, et al. Role of point shear wave elastography in the determination of the severity of fibrosis in pediatric liver diseases with pathologic correlations. J Ultrasound Med 2017;36:2337–44.



117. Dillman JR, Heider A, Bilhartz JL, Smith EA, Keshavarzi N, Rubin JM, et al. Ultrasound shear wave speed measurements correlate with liver fibrosis in children. Pediatr Radiol 2015;45:1480–8.




118. Binkovitz LA, El-Youssef M, Glaser KJ, Yin M, Binkovitz AK, Ehman RL. Pediatric MR elastography of hepatic fibrosis: principles, technique and early clinical experience. Pediatr Radiol 2012;42:402–9.




119. Hoodeshenas S, Yin M, Venkatesh SK. Magnetic resonance elastography of liver: current update. Top Magn Reson Imaging 2018;27:319–33.


120. Trout AT, Sheridan RM, Serai SD, Xanthakos SA, Su W, Zhang B, et al. Diagnostic performance of MR elastography for liver fibrosis in children and young adults with a spectrum of liver diseases. Radiology 2018;287:824–32.


121. Xanthakos SA, Podberesky DJ, Serai SD, Miles L, King EC, Balistreri WF, et al. Use of magnetic resonance elastography to assess hepatic fibrosis in children with chronic liver disease. J Pediatr 2014;164:186–8.



122. Schwimmer JB, Behling C, Angeles JE, Paiz M, Durelle J, Africa J, et al. Magnetic resonance elastography measured shear stiffness as a biomarker of fibrosis in pediatric nonalcoholic fatty liver disease. Hepatology 2017;66:1474–85.




123. Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006;43:1317–25.


124. Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003;38:518–26.


125. Adinolfi LE, Giordano MG, Andreana A, Tripodi MF, Utili R, Cesaro G, et al. Hepatic fibrosis plays a central role in the pathogenesis of thrombocytopenia in patients with chronic viral hepatitis. Br J Haematol 2001;113:590–5.



126. Aster RH. Pooling of platelets in the spleen: role in the pathogenesis of "hypersplenic" thrombocytopenia. J Clin Invest 1966;45:645–57.



127. Kamimoto Y, Horiuchi S, Tanase S, Morino Y. Plasma clearance of intravenously injected aspartate aminotransferase isozymes: evidence for preferential uptake by sinusoidal liver cells. Hepatology 1985;5:367–75.


128. GÛmez P, Coca C, Vargas C, Acebillo J, MartÌnez A. Normal referenceintervals for 20 biochemical variables in healthy infants, children, and adolescents. Clin Chem 1984;30:407–12.



129. Mercedes R, Brown J, Minard C, Tsai CM, Devaraj S, Munden M, et al. A liver biopsy validation pilot study of shear wave elastography, APRI, FIB-4, and novel serum biomarkers for liver fibrosis staging in children with chronic viral hepatitis. Glob Pediatr Health 2020;7:2333794. X20938931.




130. Shiau H, Guffey D, Loomes KM, Seidman C, Ragozzino E, Molleston JP, et al. Biopsy validated study of biomarkers for liver fibrosis and transplant prediction in inherited cholestasis. Hepatol Commun 2020;4:1516–26.




131. Alkhouri N, Mansoor S, Giammaria P, Liccardo D, Lopez R, Nobili V. The development of the pediatric NAFLD fibrosis score (PNFS) to predict the presence of advanced fibrosis in children with nonalcoholic fatty liver disease. PLoS One 2014;9:e104558.



132. Mansoor S, Collyer E, Alkhouri N. A comprehensive review of noninvasive liver fibrosis tests in pediatric nonalcoholic Fatty liver disease. Curr Gastroenterol Rep 2015;17:23.



133. Umetsu S, Inui A, Sogo T, Komatsu H, Fujisawa T. Usefulness of serum Wisteria floribunda agglutinin-positive Mac-2 binding protein in children with primary sclerosing cholangitis. Hepatol Res 2018;48:355–63.



134. Yang HR, Kim HR, Kim MJ, Ko JS, Seo JK. Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease. World J Gastroenterol 2012;18:1525–30.



135. Mosca A, Comparcola D, Romito I, Mantovani A, Nobili V, Byrne CD, et al. Plasma N-terminal propeptide of type III procollagen accurately predicts liver fibrosis severity in children with non-alcoholic fatty liver disease. Liver Int 2019;39:2317–29.



136. Hermeziu B, Messous D, Fabre M, Munteanu M, Baussan C, Bernard O, et al. Evaluation of FibroTest-ActiTest in children with chronic hepatitis C virus infection. Gastroenterol Clin Biol 2010;34:16–22.


137. El-Shabrawi MH, Mohsen NA, Sherif MM, El-Karaksy HM, Abou-Yosef H, El-Sayed HM, et al. Noninvasive assessment of hepatic fibrosis and necroinflammatory activity in Egyptian children with chronic hepatitis C virus infection using FibroTest and ActiTest. Eur J Gastroenterol Hepatol 2010;22:946–51.


138. Flores-Calderón J, Morán-Villota S, Ramón-García G, GonzálezRomano B, Bojórquez-Ramos Mdel C, Cerdán-Silva L, et al. Noninvasive markers of liver fibrosis in chronic liver disease in a group of Mexican children. A multicenter study. Ann Hepatol 2012;11:364–8.


139. de Lédinghen V, Le Bail B, Rebouissoux L, Fournier C, Foucher J, Miette V, et al. Liver stiffness measurement in children using FibroScan: feasibility study and comparison with Fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J Pediatr Gastroenterol Nutr 2007;45:443–50.


140. Pokorska-Śpiewak M, Kowalik-Mikołajewska B, Aniszewska M, Pluta M, Marczyńska M. Non-invasive evaluation of the liver disease severity in children with chronic viral hepatitis using FibroTest and ActiTest - comparison with histopathological assessment. Clin Exp Hepatol 2017;3:187–93.


141. Nobili V, Alisi A, Vania A, Tiribelli C, Pietrobattista A, Bedogni G. The pediatric NAFLD fibrosis index: a predictor of liver fibrosis in children with non-alcoholic fatty liver disease. BMC Med 2009;7:21.




142. Alkhouri N, Carter-Kent C, Lopez R, Rosenberg WM, Pinzani M, Bedogni G, et al. A combination of the pediatric NAFLD fibrosis index and enhanced liver fibrosis test identifies children with fibrosis. Clin Gastroenterol Hepatol 2011;9:150–5.


143. Alkhouri N, Sedki E, Alisi A, Lopez R, Pinzani M, Feldstein AE, et al. Combined paediatric NAFLD fibrosis index and transient elastography to predict clinically significant fibrosis in children with fatty liver disease. Liver Int 2013;33:79–85.



144. Alkhouri N. Putting it all together: Noninvasive diagnosis of fibrosis in nonalcoholic fatty liver disease in adults and children. Clin Liver Dis (Hoboken) 2017;9:134–7.




145. Gressner AM, Gao CF, Gressner OA. Non-invasive biomarkers for monitoring the fibrogenic process in liver: a short survey. World J Gastroenterol 2009;15:2433–40.



146. Ellis EL, Mann DA. Clinical evidence for the regression of liver fibrosis. J Hepatol 2012;56:1171–80.


147. Ramachandran P, Pellicoro A, Vernon MA, Boulter L, Aucott RL, Ali A, et al. Differential Ly-6C expression identifies the recruited macrophage phenotype, which orchestrates the regression of murine liver fibrosis. Proc Natl Acad Sci U S A 2012;109:E3186–95.



148. Krizhanovsky V, Yon M, Dickins RA, Hearn S, Simon J, Miething C, et al. Senescence of activated stellate cells limits liver fibrosis. Cell 2008;134:657–67.



150. Zhang J, Liu Q, He J, Li Y. Novel therapeutic targets in liver fibrosis. Front Mol Biosci 2021;8:766855.



151. Modica S, Gadaleta RM, Moschetta A. Deciphering the nuclear bile acid receptor FXR paradigm. Nucl Recept Signal 2010;8:e005.




152. Younossi ZM, Ratziu V, Loomba R, Rinella M, Anstee QM, Goodman Z, et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 2019;394:2184–96.

153. Harrison SA, Wong VW, Okanoue T, Bzowej N, Vuppalanchi R, Younes Z, et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J Hepatol 2020;73:26–39.


154. Loomba R, Lawitz E, Mantry PS, Jayakumar S, Caldwell SH, Arnold H, et al. The ASK1 inhibitor selonsertib in patients with nonalcoholic steatohepatitis: a randomized, phase 2 trial. Hepatology 2018;67:549–59.




155. Flores-Contreras L, Sandoval-Rodríguez AS, Mena-Enriquez MG, Lucano-Landeros S, Arellano-Olivera I, Álvarez-Álvarez A, et al. Treatment with pirfenidone for two years decreases fibrosis, cytokine levels and enhances CB2 gene expression in patients with chronic hepatitis C. BMC Gastroenterology 2014;14:131.




156. Aghajanian H, Kimura T, Rurik JG, Hancock AS, Leibowitz MS, Li L, et al. Targeting cardiac fibrosis with engineered T cells. Nature 2019;573:430–3.




157. Dehghani SM, Gholami S, Bahador A, Nikeghbalian S, Salahi H, Imanieh MH, et al. Morbidity and mortality of children with chronic liver diseases who were listed for liver transplantation in Iran. Pediatr Transplant 2007;11:21–3.


158. Kwong AJ, Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, et al. OPTN/SRTR 2019 Annual data report: liver. Am J Transplant 2021;21 Suppl 2:208–315.



159. Chen IY, Whitney-Miller CL, Liao X. Congenital hepatic fibrosis and its mimics: a clinicopathologic study of 19 cases at a single institution. Diagn Pathol 2021;16:81.




160. Kobelska-Dubiel N, Klincewicz B, Cichy W. Liver disease in cystic fibrosis. Prz Gastroenterol 2014;9:136–41.



161. Iorio R, Giannattasio A, Cirillo F, D' Alessandro L, Vegnente A. Longterm outcome in children with chronic hepatitis B: a 24-year observation period. Clin Infect Dis 2007;45:943–9.


163. Kendall TJ, Stedman B, Hacking N, Haw M, Vettukattill JJ, Salmon AP, et al. Hepatic fibrosis and cirrhosis in the Fontan circulation: a detailed morphological study. J Clin Pathol 2008;61:504–8.


164. Kamath BM, Ye W, Goodrich NP, Loomes KM, Romero R, Heubi JE, et al. Outcomes of childhood cholestasis in alagille syndrome: results of a multicenter observational study. Hepatol Commun 2020;4:387–98.




165. Davit-Spraul A, Gonzales E, Baussan C, Jacquemin E. Progressive familial intrahepatic cholestasis. Orphanet J Rare Dis 2009;4:1.




166. Porta G, de Carvalho E, Santos JL, Gama J, Bezerra JA. Autoimmune hepatitis: predictors of native liver survival in children and adolescents. J Pediatr 2021;229:95. –101. e3.


168. Banc-Husu AM, Bass LM. Transient elastography in pediatric liver disease. J Pediatr Gastroenterol Nutr 2021;73:141–4.


169. Trout AT, Xanthakos SA, Bennett PS, Dillman JR. Liver shear wave speed and other quantitative ultrasound measures of liver parenchyma: prospective evaluation in healthy children and adults. AJR Am J Roentgenol 2020;214:557–65.


170. Ferraioli G, De Silvestri A, Lissandrin R, Maiocchi L, Tinelli C, Filice C, et al. Evaluation of inter-system variability in liver stiffness measurements. Ultraschall Med 2019;40:64–75.


171. Galina P, Alexopoulou E, Zellos A, Grigoraki V, Siahanidou T, Kelekis NL, et al. Performance of two--dimensional ultrasound shear wave elastography: reference values of normal liver stiffness in children. Pediatr Radiol 2019;49:91–8.



172. Fraser JR, Gibson PR. Mechanisms by which food intake elevates circulating levels of hyaluronan in humans. J Intern Med 2005;258:460–6.


173. Lebensztejn DM, Wierzbicka A, Socha P, Pronicki M, Skiba E, Werpachowska I, et al. Cytokeratin-18 and hyaluronic acid levels predict liver fibrosis in children with non-alcoholic fatty liver disease. Acta Biochim Pol 2011;58:563–6.



174. Lebensztejn DM, Kaczmarski M, Sobaniec-Łotowska M, Bauer M, Voelker M, Schuppan D. Serum laminin-2 and hyaluronan predict severe liver fibrosis in children with chronic hepatitis B. Hepatology 2004;39:868–9.


175. Nobili V, Alisi A, Torre G, De Vito R, Pietrobattista A, Morino G, et al. Hyaluronic acid predicts hepatic fibrosis in children with nonalcoholic fatty liver disease. Transl Res 2010;156:229–34.


176. Hartley JL, Brown RM, Tybulewicz A, Hayes P, Wilson DC, Gillett P, et al. Hyaluronic acid predicts hepatic fibrosis in children with hepatic disease. J Pediatr Gastroenterol Nutr 2006;43:217–21.


177. Gelse K, Pöschl E, Aigner T. Collagens--structure, function, and biosynthesis. Adv Drug Deliv Rev 2003;55:1531–46.


178. Maruyama K, Okazaki I, Takagi T, Ishii H. Formation and degradation of basement membrane collagen. Alcohol Alcohol Suppl 1991;1:369–74.

179. Jarcuska P, Janicko M, Veselíny E, Jarcuska P, Skladaný L. Circulating markers of liver fibrosis progression. Clin Chim Acta 2010;411:1009–17.


180. Löhr M, Hummel F, Martus P, Cidlinsky K, Kröger JC, Hahn EG, et al. Serum levels of extracellular matrix in acute pancreatitis. Hepatogastroenterology 1999;46:3263–70.

181. van der Voort EAM, Wakkee M, Veldt-Kok P, Darwish Murad S, Nijsten T. Enhanced liver fibrosis test in patients with psoriasis, psoriatic arthritis and rheumatoid arthritis: a cross-sectional comparison with procollagen-3 N-terminal peptide (P3NP). Br J Dermatol 2017;176:1599–606.



182. Wang Y, Pan W, Zhao D, Chen Y, Chen X, Xia H. Diagnostic value of serum procollagen III N-terminal peptide for liver fibrosis in infantile cholestasis. Front Pediatr 2020;8:131.



183. Mak KM, Mei R. Basement membrane type IV collagen and laminin: an overview of their biology and value as fibrosis biomarkers of liver disease. Anat Rec (Hoboken) 2017;300:1371–90.



184. Lee CG, Da Silva CA, Dela Cruz CS, Ahangari F, Ma B, Kang MJ, et al. Role of chitin and chitinase/chitinase-like proteins in inflammation, tissue remodeling, and injury. Annu Rev Physiol 2011;73:479–501.



185. Kumagai E, Mano Y, Yoshio S, Shoji H, Sugiyama M, Korenaga M, et al. Serum YKL-40 as a marker of liver fibrosis in patients with non-alcoholic fatty liver disease. Sci Rep 2016;6:35282.




186. Lebensztejn DM, Skiba E, Werpachowska I, Sobaniec-Łotowska ME, Kaczmarski M. Serum level of YKL-40 does not predict advanced liver fibrosis in children with chronic hepatitis B. Adv Med Sci 2007;52:120–4.

187. Baeck C, Wehr A, Karlmark KR, Heymann F, Vucur M, Gassler N, et al. Pharmacological inhibition of the chemokine CCL2 (MCP-1) diminishes liver macrophage infiltration and steatohepatitis in chronic hepatic injury. Gut 2012;61:416–26.


188. Zamara E, Galastri S, Aleffi S, Petrai I, Aragno M, Mastrocola R, et al. Prevention of severe toxic liver injury and oxidative stress in MCP-1-deficient mice. J Hepatol 2007;46:230–8.


189. Lan T, Li C, Yang G, Sun Y, Zhuang L, Ou Y, et al. Sphingosine kinase 1 promotes liver fibrosis by preventing miR-19b-3p-mediated inhibition of CCR2. Hepatology 2018;68:1070–86.




190. Queck A, Bode H, Uschner FE, Brol MJ, Graf C, Schulz M, et al. Systemic MCP-1 levels derive mainly from injured liver and are associated with complications in cirrhosis. Front Immunol 2020;11:354.



191. Mühlbauer M, Bosserhoff AK, Hartmann A, Thasler WE, Weiss TS, Herfarth H, et al. A novel MCP-1 gene polymorphism is associated with hepatic MCP-1 expression and severity of HCV-related liver disease. Gastroenterology 2003;125:1085–93.


192. Chu PG, Weiss LM. Keratin expression in human tissues and neoplasms. Histopathology 2002;40:403–39.



193. Mandelia C, Collyer E, Mansoor S, Lopez R, Lappe S, Nobili V, et al. Plasma cytokeratin-18 level as a novel biomarker for liver fibrosis in children with nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr 2016;63:181–7.


194. Ikeda H, Yatomi Y, Yanase M, Satoh H, Nishihara A, Kawabata M, et al. Effects of lysophosphatidic acid on proliferation of stellate cells and hepatocytes in culture. Biochem Biophys Res Commun 1998;248:436–40.


195. Udomsinprasert W, Vejchapipat P, Klaikeaw N, Chongsrisawat V, Poovorawan Y, Honsawek S. Hepatic autotaxin overexpression in infants with biliary atresia. PeerJ 2018;6:e5224.




196. Watanabe N, Ikeda H, Nakamura K, Ohkawa R, Kume Y, Aoki J, et al. Both plasma lysophosphatidic acid and serum autotaxin levels are increased in chronic hepatitis C. J Clin Gastroenterol 2007;41:616–23.


197. Ueno T, Toyama C, Yoneyama T, Deguchi K, Nomura M, Saka R, et al. Impact of serum autotaxin level correlating with histological findings in biliary atresia. J Pediatr Surg 2021;56:1174–8.

198. Bekki Y, Yoshizumi T, Shimoda S, Itoh S, Harimoto N, Ikegami T, et al. Hepatic stellate cells secreting WFA(+) -M2BP: its role in biological interactions with Kupffer cells. J Gastroenterol Hepatol 2017;32:1387–93.








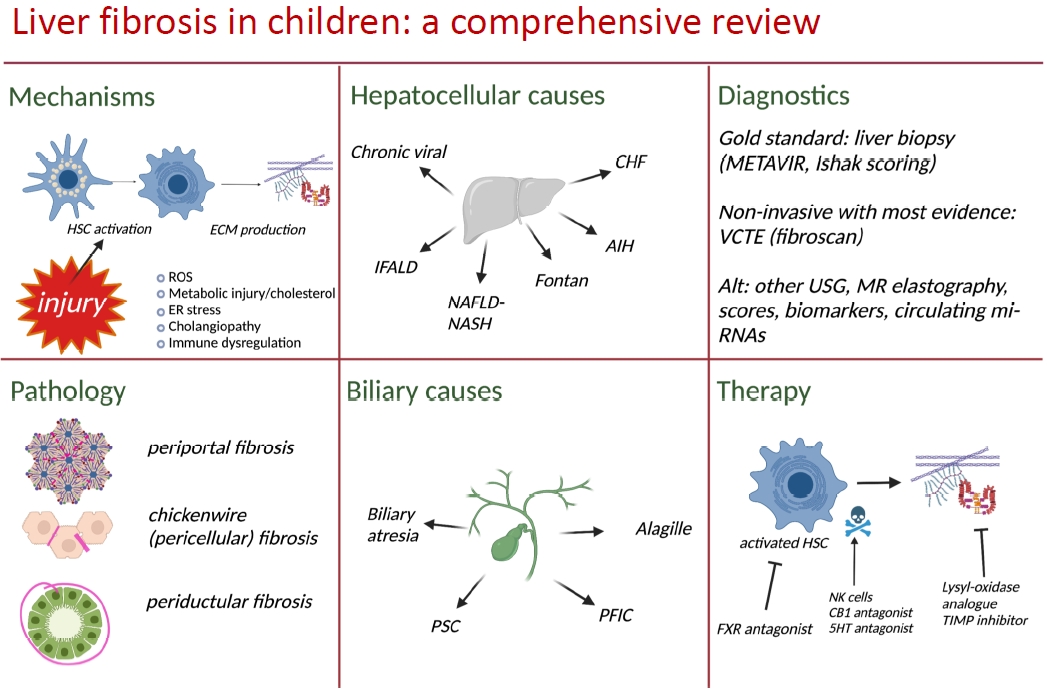
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


