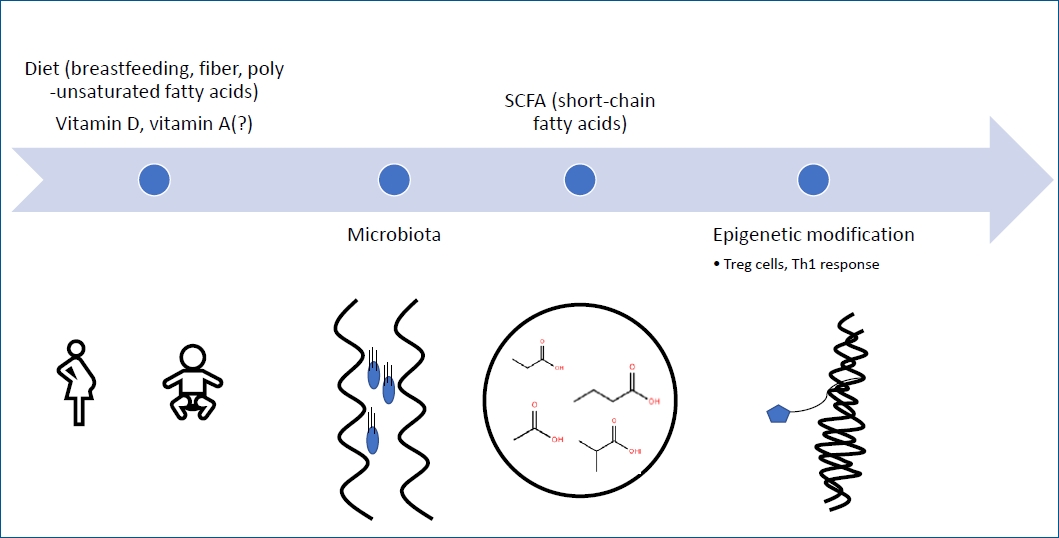
Graphical abstract
The rapidly increasing prevalence of food allergy cannot be explained by classical genetics and is therefore explained by gene-environment interactions [1]. Nutritional factors, especially during gestation and lactation, have been described as being by epigenetics mechanisms described as transmissible alterations that modify gene expression without altering the underlying DNA sequence [1,2]. Maternal nutrition, diet, and especially breastfeeding or formula feeding affect the gut microbiome, and short-chain fatty acids, one of postbiotics, which is a bacterial metabolite derived from the gut microbiota, is involved in regulatory T (Tregs) cells and Th1 immune responses [3,4]. It has also been reported that polyunsaturated fatty acids are involved in epigenetic mechanisms and T-cell maturation [5]. The diverse and abundant oligosaccharides contained in breast milk affect intestinal immune function by functioning as prebiotics that enable mitigation of Bifidobacterium et al. [6]. And secretory IgA contained in breast milk not only has a direct effect on microbial colonization, but also has a prebiotic effect that promotes the growth of certain bacterial species, affecting intestinal immune function [7]. These mechanisms suggest that breast milk is highly enriched in miRNAs, thus explaining one of the epigenetic mechanisms [8]. Vitamin D deficiency is known to affect the Th2 immune response, Treg cells, and epigenetic mechanisms by TSLP (thymic stromal lymphopoietin), an epithelial cell-derived cytokine associated with allergic diseases [9,10]. Retinoic acid, a vitamin A metabolite, acts as an important modulator and antagonist for Th9 cells, although its function in food allergy is not yet clear [11].
Methods for diagnosing food allergy include skin prick test, Immuo-CAP assay to measure allergen-specific IgE, basophil activation tests, and mast cell activation tests in addition to the gold standard double-blind placebo-controlled food challenge, bead-based epitope assays, etc. are being used, and omics approaches that can predict patients at risk of developing food allergy in the future are also being studied [12].
Recent studies have demonstrated that early introduction of peanuts, eggs, and cow's milk can lower the risk of food allergy, but further research on early introduction of other foods is needed [12].
Based on this pathophysiology, desensitization oral immunotherapy, biological agent therapy such as omalizumab, ligelizumab, dupilumab, etokimab, Bruton's tyrosine kinase inhibitor (acalabrutinib), administration of probiotics such as Lactobacillus rhamnosus GG, Bifidobacterium bifidum, and fecal microbial transplantation have been attempted [12].





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


