Introduction
Pyogenic liver abscess (PLA) occurs most frequently in persons with immunodeficiency, certain genetic disorders, infections of the skin or abdominal cavity and protein-calorie malnutrition1,2). While PLA is rare in healthy children, it may occur in immunocompetent children3). Some common organisms of PLA include Staphylococcus aureus, Streptococcus spp , Klebsiella pneumoniae, Escherichia coli, Pseudomonas aeruginosa, Salmonella and anaerobes2,4). Needle aspiration or catheter drainage of liver abscess in combination with antibiotics is the gold standard for the PLA1-3). Advances in imaging technology and techniques for drainage as well as access to new antibiotics have led to reductions in morbidity and mortality of PLA recently2). Here we describe the development of a liver abscess following K. pneumoniae infection in a 12-year-old boy who had no underlying disease. Early diagnosis with the computed tomography (CT) scans and percutaneous continuous catheter drainage at an appropriate time in combination with parenteral antibiotics were thought to be helpful, in our case.
Case report
A 12-year-old boy was admitted to Seoul St. Mary's Hospital after 5 days of fever. He had right upper quadrant (RUQ) abdominal pain when breathing for one day, but showed no other gastrointestinal symptoms such as vomiting or diarrhea. He was visiting Seoul as a tourist from Los Angeles, CA, USA. He had been healthy and had no history of any other disease; however, his grandfather had died of liver cancer related to hepatitis C. The patient had a travel history to lake about 2 weeks ago and appeared to have drunk contaminated water during swimming.
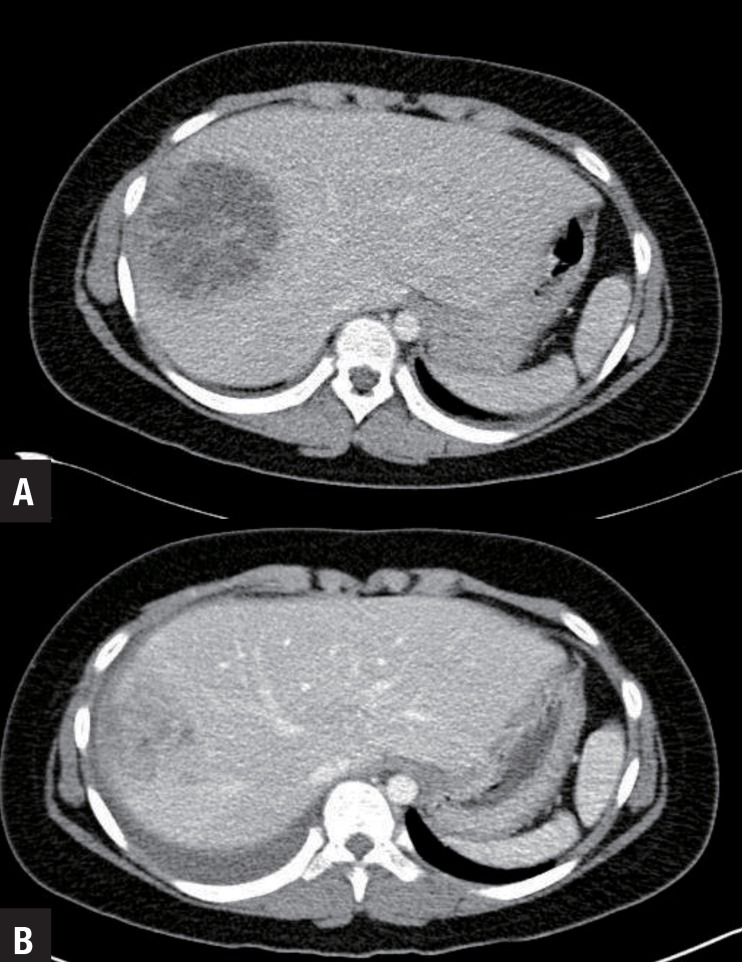
Based on physical examination, he appeared healthy. His body temperature was 39.6℃ and he had RUQ tenderness. A complete blood count showed hemoglobin, 11.7 g/dL; white blood cells, 16,810/mm3 with segmented neutrophils of 78.2%; and platelets, 270,000/mm3. The erythrocyte sedimentation rate was 120 mm/hr and his C-reactive protein was more than 34.1 mg/dL. Blood chemistry including liver function tests were normal. Abdomen and pelvis CT scans revealed a large (6.9 cm×7.1 cm×7.3 cm), lobular, low-density abscess in liver segments 7 and 8 with periportal edema and a small amount of ascites (Fig. 1A). The results of the tests for hepatitis viral markers, alpha fetoprotein, immunoglobulins, complements, and amoeba antibodies for the purpose of differential diagnosis were all normal. He was started on intravenous meropenem and metronidazole.
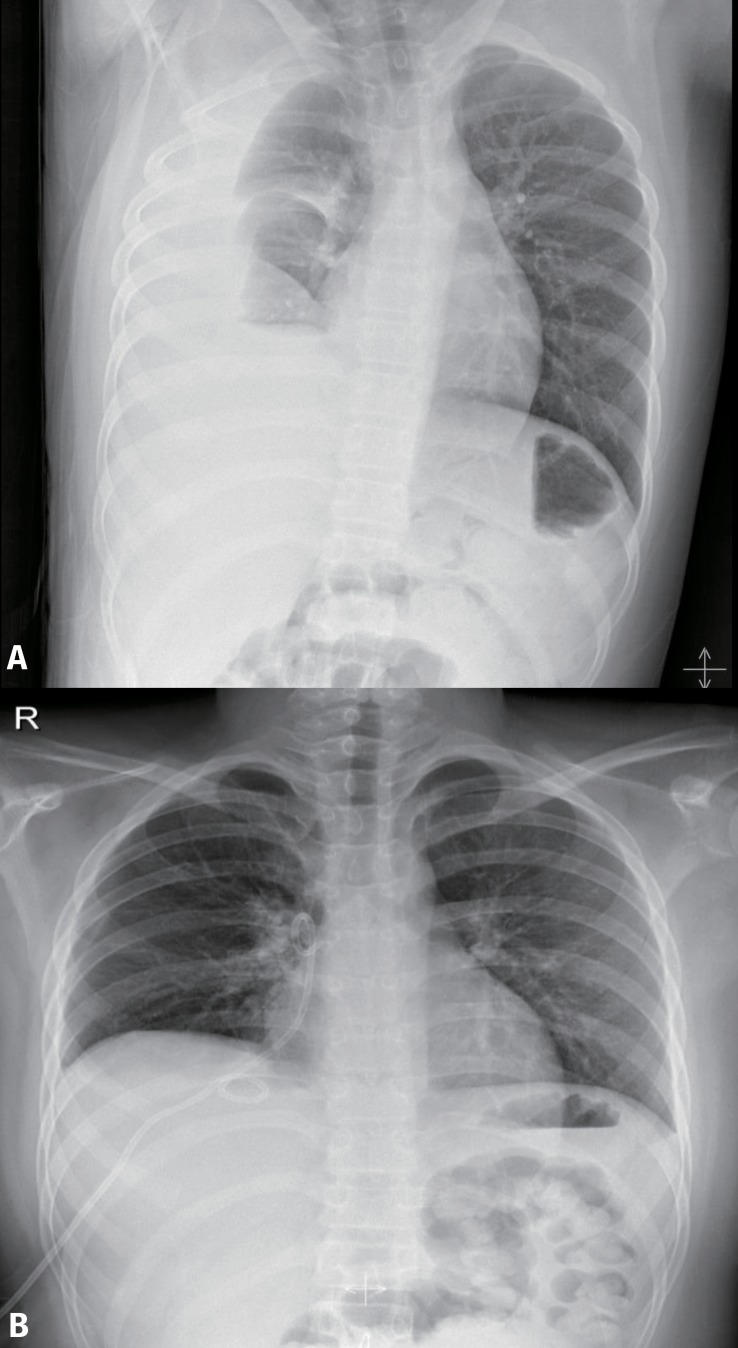
On hospital day 4, ultrasound-guided drainage was performed by pig-tail catheter, and 40 mL of pus was drained. After drainage, the patient's fever began to subside and he began to feel more comfortable. On hospital day 9, K. pneumoniae was proven by bacterial culture. The isolate was extended-spectrum beta-lactamase-negative and was sensitive to meropenem and gentamicin. We added gentamicin to initiate triple-antibiotic therapy. We removed the pig-tail catheter on hospital day 14 because the drainage had ceased. At follow-up, a repeated complete blood count showed white blood cells, 8,500/mm3 with segmented neutrophils of 58.1%; erythrocyte sedimentation rate, 113 mm/hr; and C-reactive protein, 1.71 mg/dL. On hospital day 21, abdominal and pelvic CT scans showed that the liver abscess was greatly diminished, but also showed a large amount of right pleural effusion with passive collapse of the right lower lung (Fig. 1B). Chest posterior-anterior (PA) also showed a large amount of right pleural effusion (Fig. 2A). No respiratory symptoms such as dyspnea were present. We inserted a pig-tail catheter for pleural effusion and drained 100 mL of fluid, which was shown to be transudate. The next day, as the drainage of pleural effusion ceased and chest PA showed no remaining fluid (Fig. 2B), we removed the pig-tail catheter. After treatment with intravenous antibiotics for 3 weeks (hospital day 22), we discharged the patient with oral administration of cefixime. The pleural effusion showed no evidence of bacteria in culture.
Discussion
PLA is rare in children, with an incidence of 10/100,000 hospitalizations. It can be caused by bacteria entering the liver via the portal circulation in cases of intra-abdominal infection, abscess secondary to appendicitis or inflammatory bowel disease or ascending cholangitis associated with biliary tract obstruction in immunocompetent patients. PLA occurs most frequently in immunocompromised hosts with genetic disorders, chronic granulomatous disease, diabetes or protein calorie malnutrition1-2).
The common microbiology of PLA is S. aureus, Streptococcus spp, K. pneumoniae, E. coli, P. aeruginosa, Salmonella and anaerobic organisms1,2,4). In 2003, a study in the Korean Journal of Hepatology found that K. pneumoniae is the most common organism (65.7%) causing PLA and showed a significant increase in number4). K. pneumoniae causes infections in the respiratory tract, urinary tract, lower biliary tract, and surgical wound sites5). In our case, the route of entry is probably from the gastrointestinal tract. Two hypotheses are possible yet it is difficult to explain the route of the origin. One is that K. pneumoniae was supposed to be one of carrier for our patient, the carrier rates are higher than we had expected. There is a report in Taiwan that 75% of healthy adults carry K. pneumoniae in feces6). Stool culture of the patient showed no growth but we used Hektoen enteric agar, a selective and differential agar primarily used to recover Salmonella and Shigella only. The other possibility was to get pathogen from contaminated water during swimming. The report in United States shows that K. pneumoniae is common organisms in the water, rivers, streams and lakes in the states of Oregon, Washington, and Idaho7).
Signs and symptoms are nonspecific and can include fever, nausea, vomiting, abdominal pain with RUQ tenderness, cough with breathing difficulty, and hepatomegaly3,4). On the other hand liver abscesses may present as fulminant sepsis or acute abdomen.
Laboratory testing did not have the specificity to help diagnose the PLA1). Leukocytsis and elevation of erythrocyte sedimentation rate and C-reactive protein are common. Elevations in liver function tests are common, but may also be normal.
Ultrasound or CT scans are used to confirm the diagnosis of PLA. Ultrasound is quick, safe and accurate but may miss very small abscesses or abscesses in areas of the liver that are difficult to examine with poor patient cooperation8). CT scans are more sensitive in detecting even small abscesses anywhere in the liver but have the risk of contrast nephropathy2,8). We performed CT scans the first day of hospitalization, which allowed us to make early detection. Solitary liver abscess in the right lobe is more common than multiple abscesses or solitary left lobe abscess.
Needle aspiration percutaneous continuous catheter drainage in combination with parenteral antibiotics is the gold standard treatment1,3,4,8). Antibiotic therapy should initially be broad spectrum but then narrowed, based on the culture results of the abscess fluid. The initial empirical antibiotic regimen includes ampicillin+aminoglycoside±metronidazole or vancomycin+aminoglycoside+metronidazole1,8,9). Imipenem or meropenem may also be used1,8). Others recommend a combination of a third-generation cephalosporin+metronidazol8). Antibiotic therapy is intravenous for 2-3 weeks followed by oral therapy to complete a 4-6 week course3). Advances in imaging technology and techniques for drainage as well as access to new antibiotics have led to reductions in morbidity and mortality of PLA4).
Complications of PLA include pulmonary complications, acute renal failure, peritonitis and abscess rupture, pleural effusion, pneumonia, empyema and pulmonary edema4). Common pulmonary complication in PLA include pleural effusion, pneumonia, empyema, and pulmonary edema4).
PLA is rare in children. Our patient had the typical solitary node in the right lobe and K. pneumonia was proven in bacterial culture by catheter drainage. The abscess resolved with percutaneous catheter drainage and 3 weeks of parenteral antibiotic therapy in addition to oral antibiotic therapy. Our patient developed a right pleural effusion, which resolved with subsequent drainage. He was treated well without significant complications due to early diagnosis and early drainage.



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


