Search
- Page Path
-
- HOME
- Search
- Original Article
- Hemodynamics and cerebral oxygenation in the neonatal transition: a prospective pilot study
- Daniel Pfurtscheller, Christoph Schlatzer, Nina Höller, Bernhard Schwaberger, Lukas Mileder, Nariae Baik-Schneditz, Magdalena Holter, Gerhard Pichler
-
Background: The impact of arterial blood pressure on cerebral oxygenation during immediate postnatal transition is poorly understood.
Purpose: Here we investigated the association between arterial blood pressure (BP), cerebral tissue oxygenation index (cTOI), and cerebral fractional tissue oxygen extraction (cFTOE) during the immediate postnatal transition in preterm and full-term neonates. Methods: This prospective observational study included preterm and term neonates who did... -
DOI: https://doi.org/10.3345/cep.2025.02572 [Accepted]
- Prolonged cerebral oxygenation surveillance with algorithm-based management: a neurocritical care bundle for extremely preterm infants
- Kai-Hsiang Hsu, Wei-Hung Wu, Shu-Yu Lin, Chih-Chen Chang, Mei-Yin Lai, I-Hsyuan Wu, Shih-Ming Chu, Ming-Chou Chiang, Reyin Lien
-
Background: Cerebral hypoxia-ischemia impairs brain development in extremely preterm infants and is associated with poor neurological outcomes. Near-infrared spectroscopy (NIRS) is a noninvasive continuous monitoring method for regional cerebral oxygen saturation (rcSO2).
Purpose: This study evaluated the clinical feasibility and neurological impact of a neurocritical care bundle that incorporates prolonged multidisciplinary hemodynamic monitoring and a stepwise management algorithm. Methods: Preterm infants with... -
DOI: https://doi.org/10.3345/cep.2025.02117 [Accepted]
- Perinatal risk factors for hemodynamically significant patent ductus arteriosus in very low birth weight infants
- Jie Hee Jue, So Young Shin, Jae Hyun Park, Chun Soo Kim, Hee Joung Choi
-
Background: Multiple perinatal factors influence hemodynamically significant patent ductus arteriosus (HS PDA) in preterm infants.
Purpose: This study aimed to identify the risk factors associated with HS PDA in very low birth weight infants (VLBWIs) and determine the predictors of surgical ligation. Methods: This retrospective study included VLBWIs born at 23–32 weeks’ gestation whose HS PDA properties could be identified using... -
DOI: https://doi.org/10.3345/cep.2025.01893 [Accepted]
- Global and regional burden of neonatal disorders (preterm birth, encephalopathy, jaundice, and sepsis), 1990–2021 and projections to 2050
- Yuseon Kang, Jeongseon Oh, Dongjin Yeo, Jaeyu Park, Sooji Lee, Na Yun Kim, Jungmin Park, Seung Ha Hwang, Tae Hyeong Kim, Dong Keon Yon
-
Background: Although most neonatal disorders are preventable, their global burden has not been comprehensively investigated in the context of underlying epidemiological patterns. Thus, here we conducted the first comprehensive assessment of the global burden of neonatal disorders and their 5 subtypes in 1990–2021 with projections through 2050.
Purpose: To comprehensively assess the global burden of neonatal disorders in 1990–2021 and forecast... -
DOI: https://doi.org/10.3345/cep.2025.01480 [Accepted]
- General Pediatrics
- Comparative analysis of goal attainment for helmet therapy versus conservative management for positional plagiocephaly in infants
- Bjoern Vogt, Ariane Deutschle, Georg Gosheger, Adrien Frommer, Andrea Laufer, Henning Tretow, Robert Roedl, Gregor Toporowski
- Clin Exp Pediatr. 2025;68(11):892-900. Published online October 2, 2025
-

Question: Is helmet therapy more effective than conservative management in treating positional plagiocephaly?
Finding: Both approaches reduced cranial asymmetry with comparable correction speed. Helmet therapy showed a trend toward greater severity reduction.
Meaning: Early treatment initiation was the strongest predictor of improvement. Helmet therapy may offer additional benefit in more severe cases.
- Gastroenterology
- Fecal microbiome profiles in infants with biliary atresia versus nonbiliary atresia cholestasis: a pilot study
- Nur Azizah, Fadilah Fadilah, Silvia Werdhy Lestari, Muzal Kadim, Fithriyah Sjatha, Hanifah Oswari
- Clin Exp Pediatr. 2025;68(11):932-943. Published online August 20, 2025
-

Question: How does the gut microbiota profile of infants with biliary atresia (BA) differ from that of infants with non-BA cholestasis and healthy infants in the Indonesian population?
Finding: The unique fecal microbiome composition of the BA group differed significantly from that of the other 2 groups.
Meaning: There is an urgent need to improve dysbiosis in BA and non-BA cholestasis to prevent worsening liver injury in cholestasis.
- Neonatology (Perinatology)
- Respiratory severity score-guided postnatal systemic corticosteroid therapy for bronchopulmonary dysplasia in extremely preterm infants
- Gyeong Eun Yeom, Ju Sun Heo, Baek Sup Shin, Seh Hyun Kim, Seung Han Shin, Ee-Kyung Kim, Han-Suk Kim
- Clin Exp Pediatr. 2025;68(9):656-665. Published online July 8, 2025
-

Question: Does a respiratory severity score (RSS)-guided postnatal corticosteroid protocol improve respiratory outcomes of extremely preterm (EP) infants without worsening neurodevelopmental outcomes?
Finding: The protocol enabled targeted and early steroid use, thereby reducing severe bronchopulmonary dysplasia without affecting mortality or causing neurodevelopmental impairments.
Meaning: The RSS-guided protocol may offer a more precise and individualized postnatal corticosteroid therapy for EP infants.
- General Pediatrics
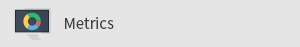
- Trends and determinants in breastfeeding among Korean infants (2007–2021): a nationwide study using the National Health Screening Program for Infants and Children
- Minwoong Kang, Eui Kyung Choi, Jeung Min Lee, Hye-Jung Shin, Woo Ryoung Lee, Son Moon Shin; Korean Society of Breastfeeding Medicine
- Clin Exp Pediatr. 2025;68(10):772-780. Published online July 4, 2025
-
Question: What are the recent trends and determinants of breastfeeding in South Korea?
Finding: Breastfeeding rates in South Korea declined significantly from 2007 to 2021, with lower rates observed in preterm, low-birthweight, and multiple-birth infants as well as rural or lower-income households.
Meaning: Targeted interventions, including prenatal education, postnatal support, and community-based programs, are required to address disparities and improve breastfeeding rates.
- Neonatology (Perinatology)
- Characterization of gut microbiota in very low birth weight infants with versus without bronchopulmonary dysplasia
- Anucha Thatrimontrichai, Manapat Praditaukrit, Gunlawadee Maneenil, Supaporn Dissaneevate, Kamonnut Singkhamanan, Komwit Surachat
- Clin Exp Pediatr. 2025;68(7):503-511. Published online February 26, 2025
-

Question: Does the gut microbiota differ between very low birth weight (VLBW) infants with versus without bronchopulmonary dysplasia (BPD)?
Finding: Common respiratory pathogens were notably elevated in the BPD group, whereas anaerobic and butyrate-producing taxa, key components of postbiotics, were dominant in the non-BPD group.
Meaning: In gut-lung communication, the interplay between the intestinal and respiratory systems may implicate pro- and postbiotics in VLBW infants with BPD.
- Review Article
- Neonatology (Perinatology)
- Recent advances in understanding pathophysiology of non-nutritional stunting in very preterm infants
- Eduardo Cuestas, Alina Rizzotti
- Clin Exp Pediatr. 2025;68(4):287-297. Published online December 23, 2024
-

· Previous reviews of extrauterine growth restriction focused mainly on weight growth restriction caused by nutritional factors or pathological conditions.
· This review summarizes recent developments in the pathophysiology of nonnutritional length growth restriction in very preterm infants with focus on the impact of sustained neonatal inflammation on their short- and long-term outcomes.
· Further research is needed to investigate optimal strategies to improve length growth restriction in very preterm infants.
- Need for national guidance regarding proactive care of infants born at 22–23 weeks' gestation
- Ga Won Jeon
- Clin Exp Pediatr. 2025;68(1):53-61. Published online November 13, 2024
-

With advancements in neonatal intensive care, the limit of viability has shifted to 22–23 weeks' gestation, whose survival rates vary across countries and institutions. These rates are not static and can be improved through the proactive and centralized care guided by national protocols, including maternal transfer to high-activity regions with better neonatal intensive care practices before delivery.
- Original Article
- Neurology
- Instability of revised Korean Developmental Screening Test classification in first year of life
- Ji Eun Jeong, You Min Kim, Na Won Lee, Gyeong Nam Kim, Jisuk Bae, Jin Kyung Kim
- Clin Exp Pediatr. 2025;68(1):97-103. Published online November 11, 2024
-

Question: How stable are the revised Korean Developmental Screening Test score classifications in early infancy?
Finding: A significant number of infants improved into the peer and high-level group (≥-1 standard deviations), especially in the gross motor area.
Meaning: The early detection of developmental delay requires a comprehensive medical history, physical and neurological examinations, and repeated developmental screenings.
- Review Article
- Neonatology (Perinatology)
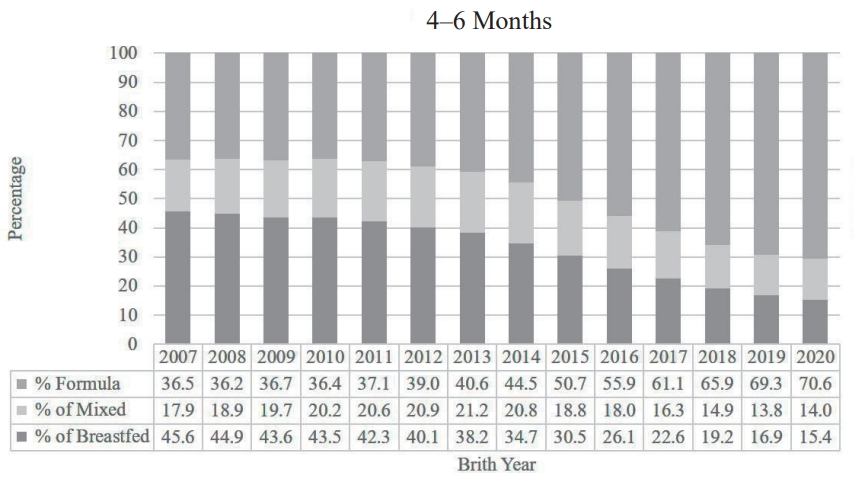
- Strategies to support language development in neonatal intensive care unit: a narrative review
- Ju Sun Heo, Ee-Kyung Kim
- Clin Exp Pediatr. 2024;67(12):651-663. Published online November 6, 2024
-
· Preterm infants often experience speech and language development delays during early childhood, impacting children's ultimate outcomes.
· Promoting breastfeeding, increasing parent-infant interactions in a single-family room, promoting a nurturing language environment by parental book reading and language interventions, and parent-integrated interventions in the neonatal intensive care unit could potentially enhance children's language development.
· Integrating these strategies through family-centered care is essential.
- Original Article
- General Pediatrics
- Effect of online infant care training and postpartum counseling based on Meleis' transition theory on mothers' readiness for care and breastfeeding: a randomized controlled trial
- Fatma Şule Bilgiç, Gülçin Bozkurt
- Clin Exp Pediatr. 2024;67(10):521-530. Published online September 27, 2024
-

Question: Do interventions based on Meleis' transition theory affect mothers' readiness for baby care and breastfeeding?
Findings: We found a statistically significant difference between the intervention and control groups in mothers' readiness for newborn care and breastfeeding (P<0.001).
Meaning: This intervention increased breastfeeding rates while ensuring that mothers were ready to care for their babies and prepared for the role of motherhood.
- Neonatology (Perinatology)
- Mortality of very low birth weight infants by neonatal intensive care unit workload and regional group status
- Sung-Hoon Chung, Chae Young Kim, Yong-Sung Choi, Myung Hee Lee, Jae Woo Lim, Byong Sop Lee, Ki-Soo Kim; the Korean Neonatal Network
- Clin Exp Pediatr. 2024;67(11):619-627. Published online September 12, 2024
-

Question: How do structural and staffing characteristics of neonatal intensive care units (NICUs) influence the mortality rates of very low birth weight infants (VLBWIs)?
Findings: NICUs with higher staffing levels, particularly with more neonatologists, and those offering advanced care levels were associated with lower mortality rates. Additionally, regional disparities were observed, with some areas demon-strating significantly higher survival rates.
Meaning: Adequate staffing and equitable regional distribution of medical resources are crucial for improving survival outcomes in VLBWIs. Efforts to enhance NICU staffing and address regional healthcare disparities are essential for optimizing care quality and reducing mortality in this vulnerable population.
- Developmental and Behavioral Medicine
- Effectiveness of online responsive teaching in young children with developmental disabilities: a pilot study
- Jung Sook Yeom, Jeongmee Kim
- Clin Exp Pediatr. 2024;67(6):303-311. Published online May 21, 2024
-

Question: Does online responsive teaching (RT) impact children's and parents’ emotions and behaviors, and do parents find it satisfactory?
Finding: Online RT significantly improved children's pivotal and problem behaviors, decreased parenting stress, and enhanced parental interactive styles with high satisfaction.
Meaning: This pilot study's findings suggest that online RT can enhance child outcomes, offering accessible interventions amid challenges such as limited access and pandemics.
- Neonatology (Perinatology)
- Effect of vitamin E supplementation on bilirubin levels in infants with hyperbilirubinemia: a double-blind randomized clinical trial
- Mojtaba Cheraghi, Maziar Nikouei, Majid Mansouri, Siros Hemmatpour, Yousef Moradi
- Clin Exp Pediatr. 2024;67(5):249-256. Published online March 26, 2024
-
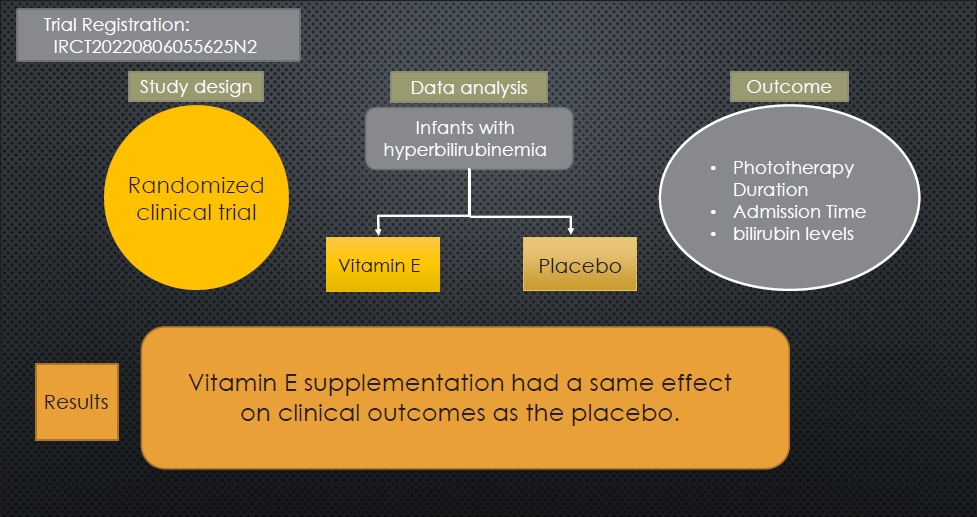
Question: Is vitamin E a viable therapeutic option for managing neonatal hyperbilirubinemia?
Finding: This randomized clinical trial examined the effects of oral vitamin E supplementation on bilirubin reduction (primary outcome), phototherapy duration, and length of hospital stay (secondary outcome) in 138 infants.
Meaning: Infants administered vitamin E versus placebo demonstrated similar reductions in bilirubin levels and length of hospital stay.
- Review Article
- Infection
- COVID-19 among infants: key clinical features and remaining controversies
- Nevio Cimolai
- Clin Exp Pediatr. 2024;67(1):1-16. Published online November 27, 2023
-
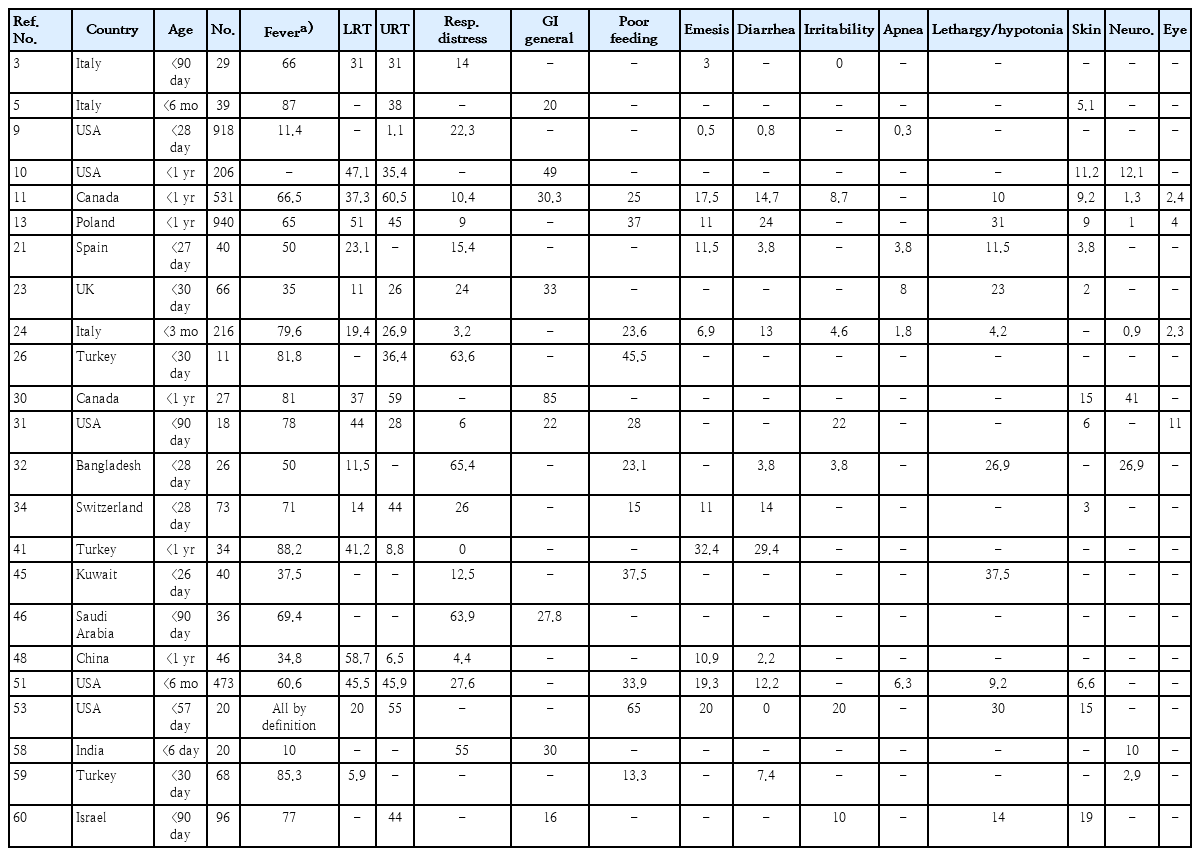
· Clinical studies of coronavirus disease 2019 (COVID-19) in infants should be supported by rigorous laboratory diagnostic criteria.
· Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spreads to infants similarly to other viral respiratory infections.
· Among infants ≤1 year of age beyond the immediate postpartum period, COVID-19 is relatively mild, but even the low risk of severe disease requires prevention.
· Comorbidities increase infection vulnerability and complications in infants.
· Clinical and laboratory data do not sufficiently distinguish COVID-19 from other respiratory viral infections.
· Coinfection with SARS-CoV-2 is uncommon among infants.
· Unique infection sequelae, including multi-inflammatory syndrome in children and neonates and long COVID require further study and refinement of diagnostic criteria.
· Infection control standards applied to mother-infant dyads should be tempered by standard preventive strategies, maternal input, accommodation potential, and overall safety.
· Maternal vaccination prevents disease in early infancy.
- Neonatology (Perinatology)
- Influence of infant microbiome on health and development
- Noelle Younge
- Clin Exp Pediatr. 2024;67(5):224-231. Published online August 21, 2023
-

· The infant gut microbiome is highly dynamic and individualized.
· Microbes are vertically transmitted from mother to infant during delivery and throughout infancy.
· Delivery mode, gestational age, diet, and antibiotic use influence infant microbiome composition and function.
· In animal studies, the microbiome played critical roles in the structural and functional development of the infant gastrointestinal and immune systems.
· Microbiome-targeted therapies have great potential to reduce infant morbidity and mortality.
- Updates in neonatal resuscitation: routine use of laryngeal masks as an alternative to face masks
- Eun Song Song, Ga Won Jeon
- Clin Exp Pediatr. 2024;67(5):240-246. Published online July 11, 2023
-

In neonatal resuscitation:
· Laryngeal masks are recommended when endotracheal intubation or positive-pressure ventilation fails.
· Laryngeal masks are useful even during chest compressions.
· Laryngeal masks aid neonates >34 weeks’ gestation and/or with a birth weight >2 kg.
· Main usage barriers include limited experience (81%), preference for endotracheal tubes (57%), and lack of awareness (56%).
· Second-generation laryngeal masks have a built-in esophageal drainage tube that prevents regurgitation into the glottis, and an orogastric tube can be inserted within the esophageal drainage tube to protect against gastric inflation.
- Neonatal family-centered care: evidence and practice models
- Juyoung Lee
- Clin Exp Pediatr. 2024;67(4):171-177. Published online June 14, 2023
-
· Concrete evidence exists of early parent-infant attachment supported by family-centered care (FCC) in the neonatal intensive care unit.
· FCC involves the parents’ presence and participation in the infant’s care and decision-making.
· A private and comfortable space should be provided. A single-family room is ideal; however, a quiet space with a recliner can be a good alternative.
· Care culture changes and staff training are required.
- Original Article
- Neurology
- Need for palliative care from birth to infancy in pediatric patients with neurological diseases
- Raffaele Falsaperla, Silvia Marino, Carla Moscheo, Lucia Giovanna Tardino, Simona Domenica Marino, Concetta Sciuto, Piero Pavone, Giovanna Vitaliti, Federica Sullo, Martino Ruggieri
- Clin Exp Pediatr. 2023;66(8):350-356. Published online June 14, 2023
-
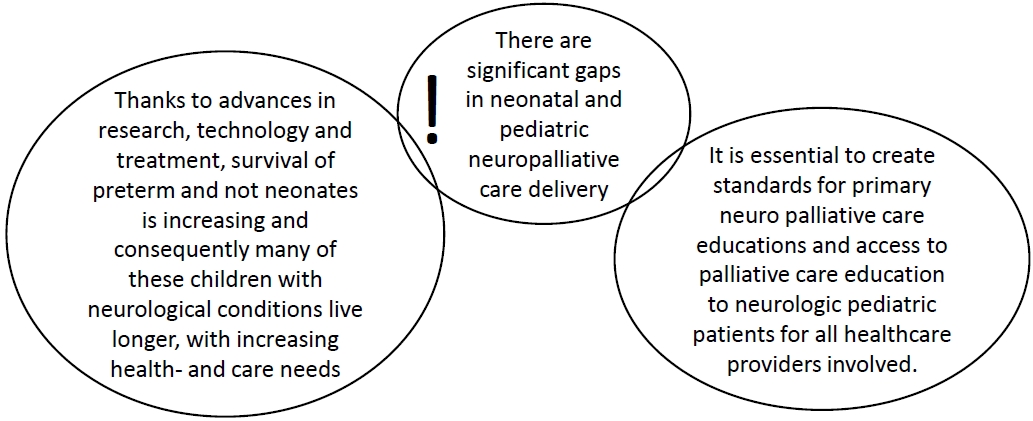
Question: What are the current palliative care protocols, palliative course, and implementable palliative care programs for hospitalized pediatric patients with neurological diseases in Italy?
Finding: We studied 34 newborns with nervous system diseases, all of whom had a poor prognosis.
Meaning: Despite current legislation in Italy, no palliative care network has been implemented. Given the vast number of patients with neurological conditions, standardized palliative care guidelines and protocols are required.
- Developmental and Behavioral Medicine
- Parenting stress and interactive engagement behaviors in children with developmental delay
- Jung Sook Yeom, Rock Bum Kim, Jae Young Cho, Ji Sook Park, Eun Sil Park, Ji-Hyun Seo, Jae-Young Lim, Hyang-Ok Woo
- Clin Exp Pediatr. 2023;66(6):252-261. Published online May 19, 2023
-
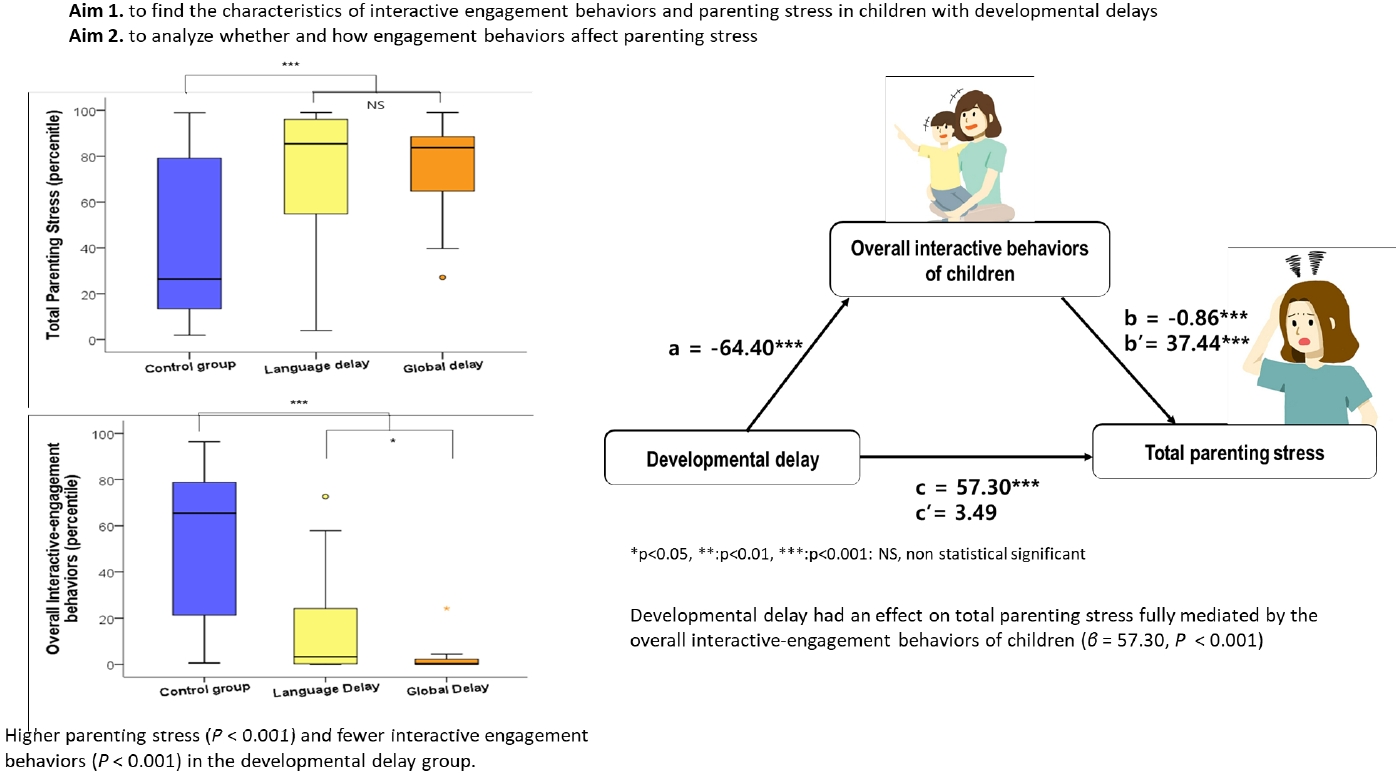
· Question: What level of parenting stress is experienced by parents of children with developmental delays (DDs) without autism spectrum disorder, and what factors contribute to it?
· Findings: Parents of children with DDs experienced high parenting stress that were significantly mediated by their children’s low interactive behaviors.
· Meaning: The interactive behaviors of children with DDs mediate parenting stress.
- Review Article
- Other
- Hearing loss in neonates and infants
- Goun Choe, Su-Kyoung Park, Bong Jik Kim
- Clin Exp Pediatr. 2023;66(9):369-376. Published online January 9, 2023
-
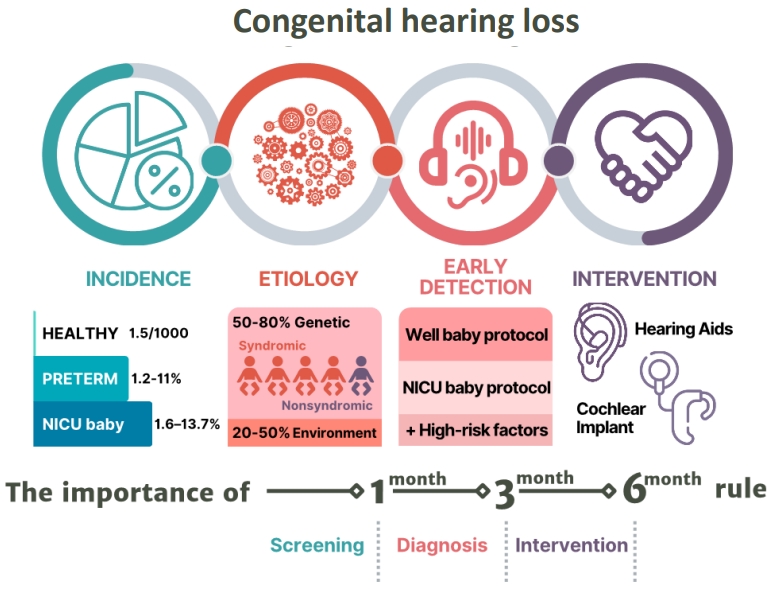
· Congenital hearing loss is common, with an approximate incidence of 1.5 per 1,000 newborns and affecting 1.2%–11% of preterm and 1.6%–13.7% of neonatal intensive care unit neonates.
· Etiologies vary, and up to 80% of cases are genetic.
· Newborn hearing screenings follow the 1-3-6 rule, and babies at high risk of hearing loss should be referred to otolaryngology for early detection and timely intervention.
- Neonatology (Perinatology)
- Neurodevelopmental outcomes of preterm infants
- In Gyu Song
- Clin Exp Pediatr. 2023;66(7):281-287. Published online December 30, 2022
-

· Among survivors, 60.9% of infants born at 22 weeks’ gestation had moderate to severe impairments, whereas 50.3% born at 23 weeks’ and 42.2% at 24 weeks’ gestation had moderate to severe impairments.
· Moderate and late preterm infants reportedly have less severe disease than very preterm infants, but they still experience adverse neurodevelopmental outcomes.
· The careful follow-up and early detection of developmental problems in these patients are required.
- Original Article
- Neonatology (Perinatology)
- A thickened formula reduces feeding-associated oxygen desaturation and bradycardia in preterm infants
- Gayoung Lee, Juyoung Lee, Ga Won Jeon, Yong Hoon Jun
- Clin Exp Pediatr. 2023;66(1):32-37. Published online December 15, 2022
-
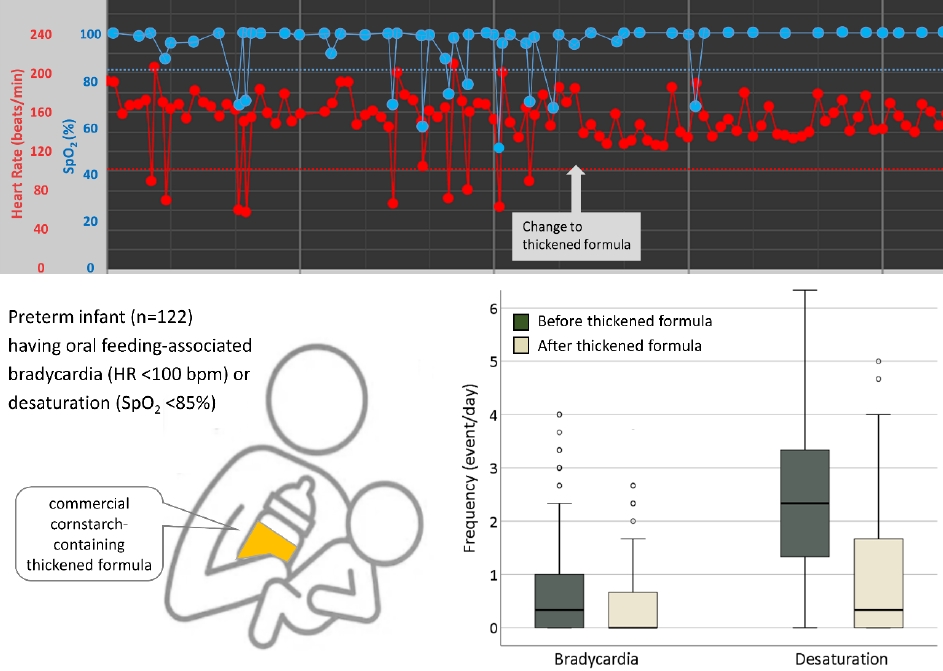
Question: Is a commercial thickened formula able to alleviate oral feeding-associated desaturation and bradycardia in preterm infants?
Finding: Thickened formula feeding significantly reduced oral feeding-associated desaturation and bradycardia in preterm infants.
Meaning: Thickened formula feeding stabilizes oxygen saturation and heart rate during oral feeding among preterm infants with feeding difficulties.
- Gastroenterology
- Probiotics added to maternal nutrition affect ınfantile colic symptoms and fecal microbiota profile: a single-blind randomized controlled study
- Aysu Yıldız Karaahmet, Gülümser Dolgun, Metehan Özen
- Clin Exp Pediatr. 2022;65(11):547-554. Published online September 23, 2022
-

Question: Do probiotics added to maternal nutrition affect infantile colic symptoms and intestinal microbiota?
Finding: Infants whose mothers ingested probiotics demonstrated decreased crying frequency and intensity and significantly increased bacterial diversity in the stools. The bacterial variety was substantially affected by the added probiotic product.
Meaning: The addition of probiotics to maternal nutrition in early infancy could play an important role in preventing infantile colic.
- Review Article
- Nephrology (Genitourinary)
- Neonatal hypertension: concerns within and beyond the neonatal intensive care unit
- Kathleen Altemose, Janis M. Dionne
- Clin Exp Pediatr. 2022;65(8):367-376. Published online May 30, 2022
-
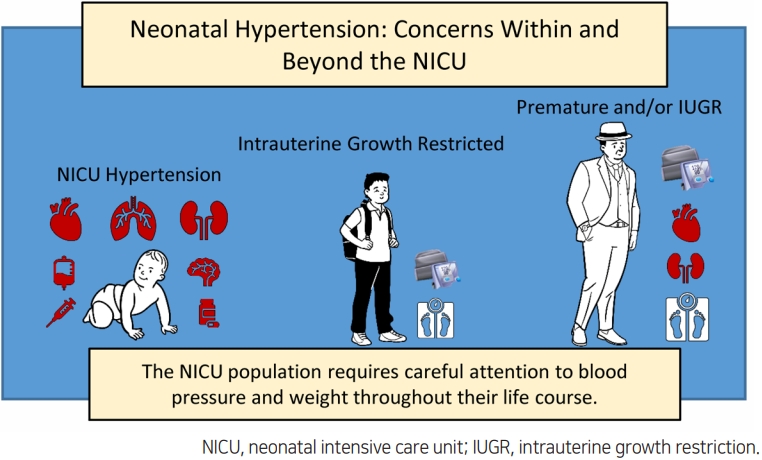
Some neonates, especially those who are premature, may experience hypertension while in the neonatal intensive care unit (NICU). The most common causes are prematurity-related and the hypertension usually resolves over the first 1–2 years of life. Unfortunately, the increasing population of NICU graduates is at risk for later cardiovascular and kidney disease in childhood and adulthood. This population requires careful attention to blood pressure and weight throughout their life course.
- Original Article
- Other
- Plastic bottle feeding produces changes in biochemical parameters in human infants – A pilot study
- Mahendra K. Pant, Abul. H. Ahmad, Manisha Naithani, Jayanti Pant
- Clin Exp Pediatr. 2022;65(9):459-465. Published online May 19, 2022
-

Question: Plastic feeding bottles are used commonly to feed infants who cannot be breastfeed. Does plastic bottle feeding produce biochemical changes in infants?
Finding: The plastic bottles leach out endocrine disruptors and affects bodily functions in terms of biochemical alterations like increased blood urea, raised creatine-kinase–MB levels, and altered lipid profile in infants exposed to bottle feeding.
Meaning: Plastic bottles feeding alters bodily functions in infants.
- Review Article
- Gastroenterology
- Clinical importance of immunonutrition in infants: a review of the recent literature
- Ji Sook Park
- Clin Exp Pediatr. 2022;65(7):337-343. Published online February 17, 2022
-

Nutrients are important in the developing immune system. Human milk supplies diverse bioactives to prevent acute infection or chronic inflammation. Immunoglobulins, lactoferrin, and glutamine in human milk decrease gastrointestinal and respiratory infection. Human milk oligosaccharides promote the growth of intestinal microbiota, the gut barrier, and antimicrobial or antiviral activity. Micronutrients act as anti-inflammatory immunonutrients, too. However, the toxicity of some nutrients from an overdose should be considered.
-

-
-
6.02024CiteScore98th percentilePowered by
-
Impact Factor3.6
-
- TOPICS
- ARTICLE CATEGORY
- Editorial Office
-
Korean Pediatric Society
#1606 Seocho World Officetel, 19 Seoun-ro, Seocho-ku, Seoul 06732, Korea
Tel: +82-2-3473-7306 Fax: +82-2-3473-7307 E-mail: office@e-cep.org
Clinical and Experimental Pediatrics is an open access journal. All articles are distributed under the terms of the Creative Commons Attribution NonCommercial License (http://creativecommons.org/licenses/by-nc/4.0/)
Copyright © 2026 by Korean Pediatric Society.