Search
- Page Path
-
- HOME
- Search
- Original Article
- Neonatology (Perinatology)
- Characterization of gut microbiota in very low birth weight infants with versus without bronchopulmonary dysplasia
- Anucha Thatrimontrichai, Manapat Praditaukrit, Gunlawadee Maneenil, Supaporn Dissaneevate, Kamonnut Singkhamanan, Komwit Surachat
- Clin Exp Pediatr. 2025;68(7):503-511. Published online February 26, 2025
-

Question: Does the gut microbiota differ between very low birth weight (VLBW) infants with versus without bronchopulmonary dysplasia (BPD)?
Finding: Common respiratory pathogens were notably elevated in the BPD group, whereas anaerobic and butyrate-producing taxa, key components of postbiotics, were dominant in the non-BPD group.
Meaning: In gut-lung communication, the interplay between the intestinal and respiratory systems may implicate pro- and postbiotics in VLBW infants with BPD.
- Review Article
- Neonatology (Perinatology)
- Recent advances in understanding pathophysiology of non-nutritional stunting in very preterm infants
- Eduardo Cuestas, Alina Rizzotti
- Clin Exp Pediatr. 2025;68(4):287-297. Published online December 23, 2024
-

· Previous reviews of extrauterine growth restriction focused mainly on weight growth restriction caused by nutritional factors or pathological conditions.
· This review summarizes recent developments in the pathophysiology of nonnutritional length growth restriction in very preterm infants with focus on the impact of sustained neonatal inflammation on their short- and long-term outcomes.
· Further research is needed to investigate optimal strategies to improve length growth restriction in very preterm infants.
- Need for national guidance regarding proactive care of infants born at 22–23 weeks' gestation
- Ga Won Jeon
- Clin Exp Pediatr. 2025;68(1):53-61. Published online November 13, 2024
-

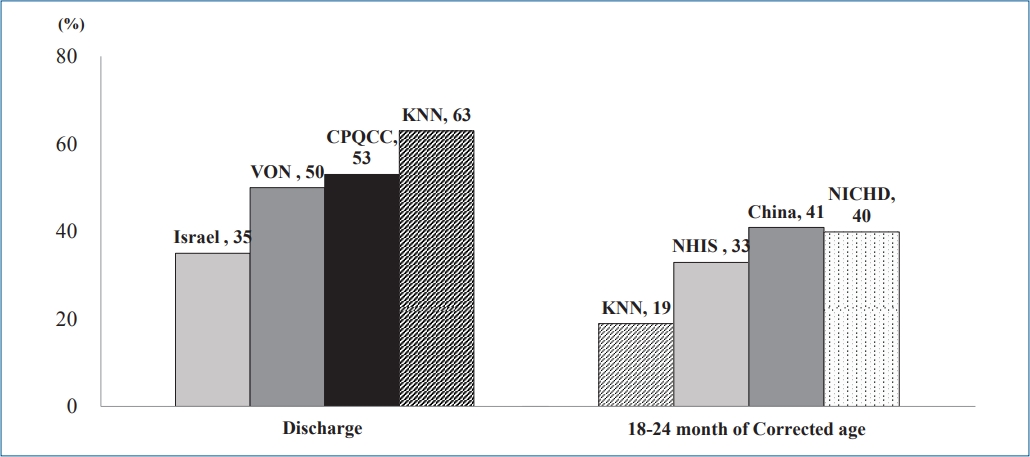
With advancements in neonatal intensive care, the limit of viability has shifted to 22–23 weeks' gestation, whose survival rates vary across countries and institutions. These rates are not static and can be improved through the proactive and centralized care guided by national protocols, including maternal transfer to high-activity regions with better neonatal intensive care practices before delivery.
- Original Article
- Neurology
- Instability of revised Korean Developmental Screening Test classification in first year of life
- Ji Eun Jeong, You Min Kim, Na Won Lee, Gyeong Nam Kim, Jisuk Bae, Jin Kyung Kim
- Clin Exp Pediatr. 2025;68(1):97-103. Published online November 11, 2024
-

Question: How stable are the revised Korean Developmental Screening Test score classifications in early infancy?
Finding: A significant number of infants improved into the peer and high-level group (≥-1 standard deviations), especially in the gross motor area.
Meaning: The early detection of developmental delay requires a comprehensive medical history, physical and neurological examinations, and repeated developmental screenings.
- Review Article
- Neonatology (Perinatology)
- Strategies to support language development in neonatal intensive care unit: a narrative review
- Ju Sun Heo, Ee-Kyung Kim
- Clin Exp Pediatr. 2024;67(12):651-663. Published online November 6, 2024
-
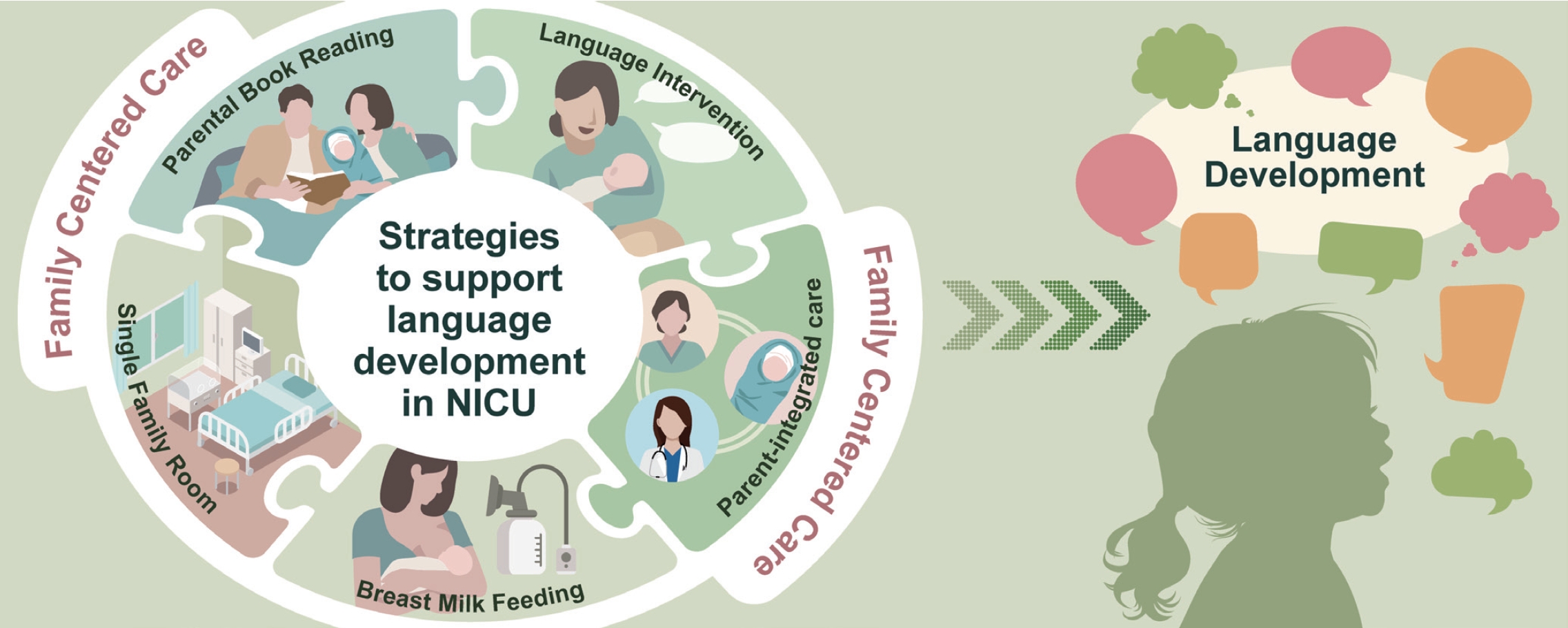
· Preterm infants often experience speech and language development delays during early childhood, impacting children's ultimate outcomes.
· Promoting breastfeeding, increasing parent-infant interactions in a single-family room, promoting a nurturing language environment by parental book reading and language interventions, and parent-integrated interventions in the neonatal intensive care unit could potentially enhance children's language development.
· Integrating these strategies through family-centered care is essential.
- Original Article
- General Pediatrics
- Effect of online infant care training and postpartum counseling based on Meleis' transition theory on mothers' readiness for care and breastfeeding: a randomized controlled trial
- Fatma Şule Bilgiç, Gülçin Bozkurt
- Clin Exp Pediatr. 2024;67(10):521-530. Published online September 27, 2024
-

Question: Do interventions based on Meleis' transition theory affect mothers' readiness for baby care and breastfeeding?
Findings: We found a statistically significant difference between the intervention and control groups in mothers' readiness for newborn care and breastfeeding (P<0.001).
Meaning: This intervention increased breastfeeding rates while ensuring that mothers were ready to care for their babies and prepared for the role of motherhood.
- Neonatology (Perinatology)
- Mortality of very low birth weight infants by neonatal intensive care unit workload and regional group status
- Sung-Hoon Chung, Chae Young Kim, Yong-Sung Choi, Myung Hee Lee, Jae Woo Lim, Byong Sop Lee, Ki-Soo Kim; the Korean Neonatal Network
- Clin Exp Pediatr. 2024;67(11):619-627. Published online September 12, 2024
-

Question: How do structural and staffing characteristics of neonatal intensive care units (NICUs) influence the mortality rates of very low birth weight infants (VLBWIs)?
Findings: NICUs with higher staffing levels, particularly with more neonatologists, and those offering advanced care levels were associated with lower mortality rates. Additionally, regional disparities were observed, with some areas demon-strating significantly higher survival rates.
Meaning: Adequate staffing and equitable regional distribution of medical resources are crucial for improving survival outcomes in VLBWIs. Efforts to enhance NICU staffing and address regional healthcare disparities are essential for optimizing care quality and reducing mortality in this vulnerable population.
- Developmental and Behavioral Medicine
- Effectiveness of online responsive teaching in young children with developmental disabilities: a pilot study
- Jung Sook Yeom, Jeongmee Kim
- Clin Exp Pediatr. 2024;67(6):303-311. Published online May 21, 2024
-

Question: Does online responsive teaching (RT) impact children's and parents’ emotions and behaviors, and do parents find it satisfactory?
Finding: Online RT significantly improved children's pivotal and problem behaviors, decreased parenting stress, and enhanced parental interactive styles with high satisfaction.
Meaning: This pilot study's findings suggest that online RT can enhance child outcomes, offering accessible interventions amid challenges such as limited access and pandemics.
- Neonatology (Perinatology)
- Effect of vitamin E supplementation on bilirubin levels in infants with hyperbilirubinemia: a double-blind randomized clinical trial
- Mojtaba Cheraghi, Maziar Nikouei, Majid Mansouri, Siros Hemmatpour, Yousef Moradi
- Clin Exp Pediatr. 2024;67(5):249-256. Published online March 26, 2024
-
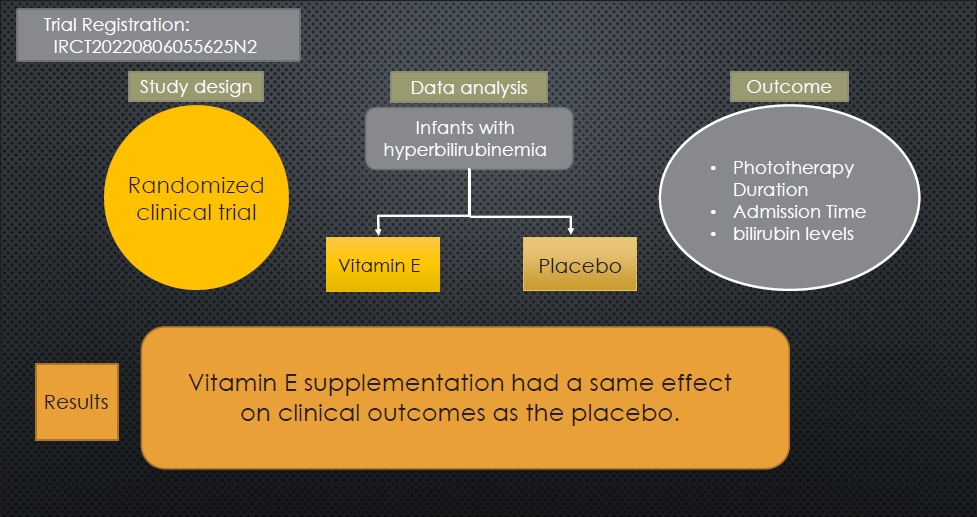
Question: Is vitamin E a viable therapeutic option for managing neonatal hyperbilirubinemia?
Finding: This randomized clinical trial examined the effects of oral vitamin E supplementation on bilirubin reduction (primary outcome), phototherapy duration, and length of hospital stay (secondary outcome) in 138 infants.
Meaning: Infants administered vitamin E versus placebo demonstrated similar reductions in bilirubin levels and length of hospital stay.
- Review Article
- Infection
- COVID-19 among infants: key clinical features and remaining controversies
- Nevio Cimolai
- Clin Exp Pediatr. 2024;67(1):1-16. Published online November 27, 2023
-
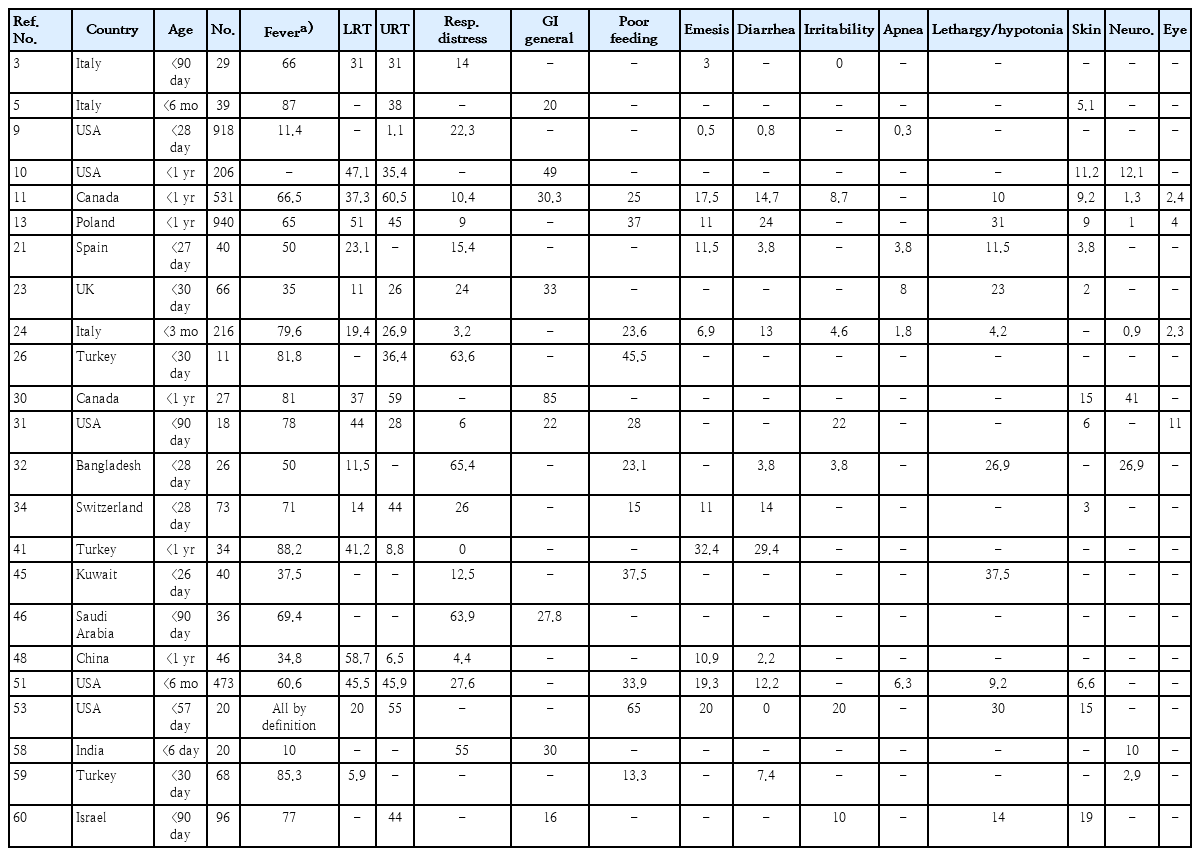
· Clinical studies of coronavirus disease 2019 (COVID-19) in infants should be supported by rigorous laboratory diagnostic criteria.
· Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spreads to infants similarly to other viral respiratory infections.
· Among infants ≤1 year of age beyond the immediate postpartum period, COVID-19 is relatively mild, but even the low risk of severe disease requires prevention.
· Comorbidities increase infection vulnerability and complications in infants.
· Clinical and laboratory data do not sufficiently distinguish COVID-19 from other respiratory viral infections.
· Coinfection with SARS-CoV-2 is uncommon among infants.
· Unique infection sequelae, including multi-inflammatory syndrome in children and neonates and long COVID require further study and refinement of diagnostic criteria.
· Infection control standards applied to mother-infant dyads should be tempered by standard preventive strategies, maternal input, accommodation potential, and overall safety.
· Maternal vaccination prevents disease in early infancy.
- Neonatology (Perinatology)
- Influence of infant microbiome on health and development
- Noelle Younge
- Clin Exp Pediatr. 2024;67(5):224-231. Published online August 21, 2023
-

· The infant gut microbiome is highly dynamic and individualized.
· Microbes are vertically transmitted from mother to infant during delivery and throughout infancy.
· Delivery mode, gestational age, diet, and antibiotic use influence infant microbiome composition and function.
· In animal studies, the microbiome played critical roles in the structural and functional development of the infant gastrointestinal and immune systems.
· Microbiome-targeted therapies have great potential to reduce infant morbidity and mortality.
- Updates in neonatal resuscitation: routine use of laryngeal masks as an alternative to face masks
- Eun Song Song, Ga Won Jeon
- Clin Exp Pediatr. 2024;67(5):240-246. Published online July 11, 2023
-

In neonatal resuscitation:
· Laryngeal masks are recommended when endotracheal intubation or positive-pressure ventilation fails.
· Laryngeal masks are useful even during chest compressions.
· Laryngeal masks aid neonates >34 weeks’ gestation and/or with a birth weight >2 kg.
· Main usage barriers include limited experience (81%), preference for endotracheal tubes (57%), and lack of awareness (56%).
· Second-generation laryngeal masks have a built-in esophageal drainage tube that prevents regurgitation into the glottis, and an orogastric tube can be inserted within the esophageal drainage tube to protect against gastric inflation.
- Neonatal family-centered care: evidence and practice models
- Juyoung Lee
- Clin Exp Pediatr. 2024;67(4):171-177. Published online June 14, 2023
-
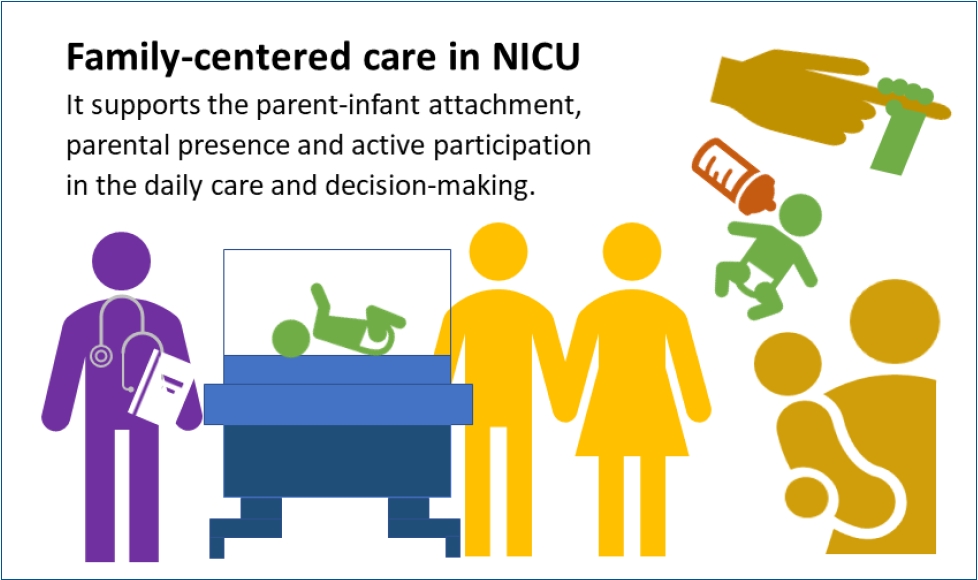
· Concrete evidence exists of early parent-infant attachment supported by family-centered care (FCC) in the neonatal intensive care unit.
· FCC involves the parents’ presence and participation in the infant’s care and decision-making.
· A private and comfortable space should be provided. A single-family room is ideal; however, a quiet space with a recliner can be a good alternative.
· Care culture changes and staff training are required.
- Original Article
- Neurology
- Need for palliative care from birth to infancy in pediatric patients with neurological diseases
- Raffaele Falsaperla, Silvia Marino, Carla Moscheo, Lucia Giovanna Tardino, Simona Domenica Marino, Concetta Sciuto, Piero Pavone, Giovanna Vitaliti, Federica Sullo, Martino Ruggieri
- Clin Exp Pediatr. 2023;66(8):350-356. Published online June 14, 2023
-
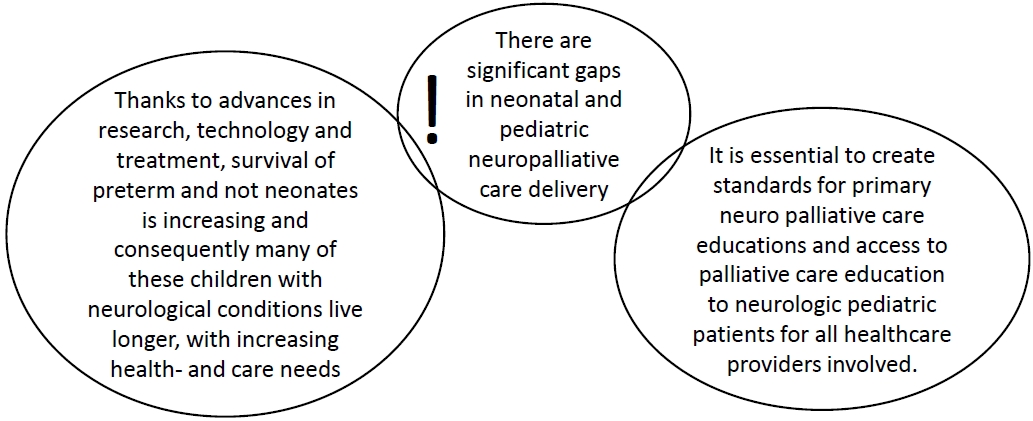
Question: What are the current palliative care protocols, palliative course, and implementable palliative care programs for hospitalized pediatric patients with neurological diseases in Italy?
Finding: We studied 34 newborns with nervous system diseases, all of whom had a poor prognosis.
Meaning: Despite current legislation in Italy, no palliative care network has been implemented. Given the vast number of patients with neurological conditions, standardized palliative care guidelines and protocols are required.
- Developmental and Behavioral Medicine
- Parenting stress and interactive engagement behaviors in children with developmental delay
- Jung Sook Yeom, Rock Bum Kim, Jae Young Cho, Ji Sook Park, Eun Sil Park, Ji-Hyun Seo, Jae-Young Lim, Hyang-Ok Woo
- Clin Exp Pediatr. 2023;66(6):252-261. Published online May 19, 2023
-
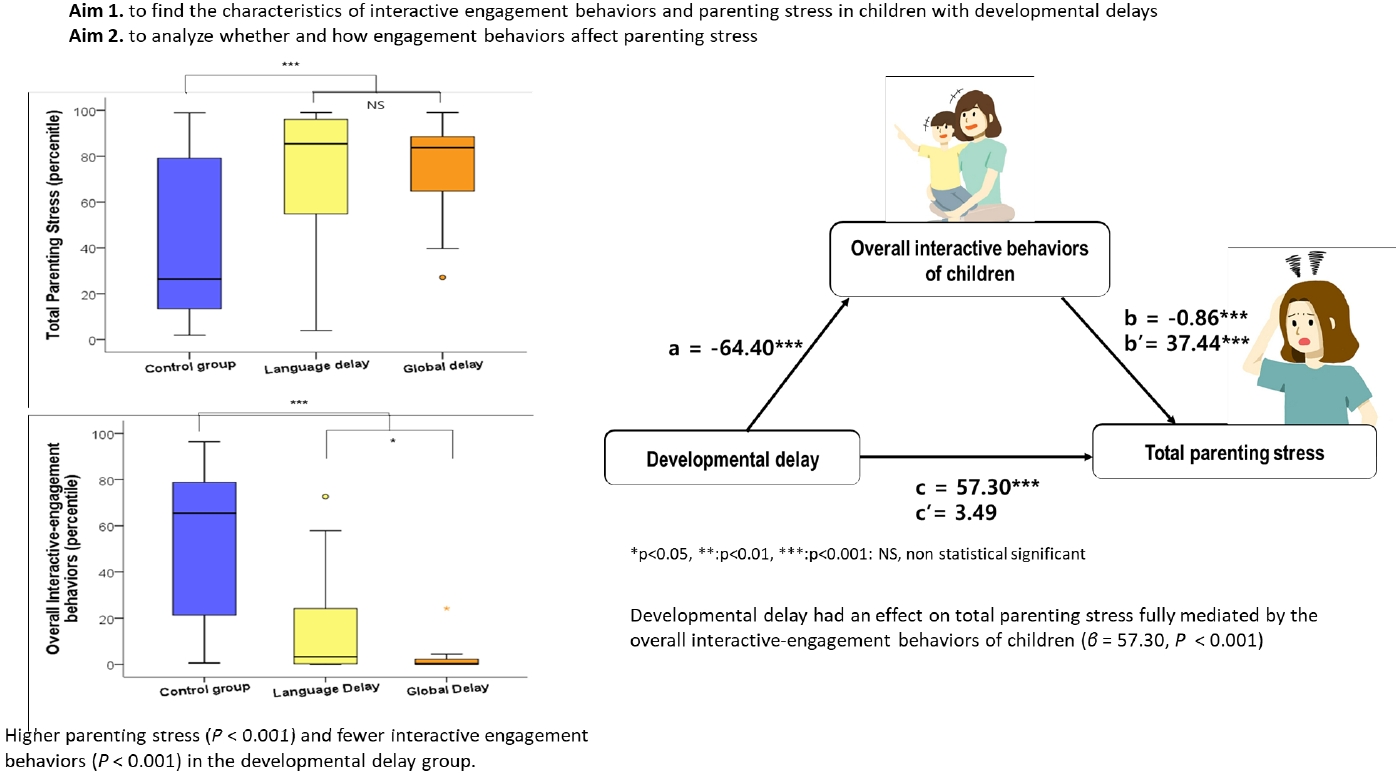
· Question: What level of parenting stress is experienced by parents of children with developmental delays (DDs) without autism spectrum disorder, and what factors contribute to it?
· Findings: Parents of children with DDs experienced high parenting stress that were significantly mediated by their children’s low interactive behaviors.
· Meaning: The interactive behaviors of children with DDs mediate parenting stress.
- Review Article
- Other
- Hearing loss in neonates and infants
- Goun Choe, Su-Kyoung Park, Bong Jik Kim
- Clin Exp Pediatr. 2023;66(9):369-376. Published online January 9, 2023
-
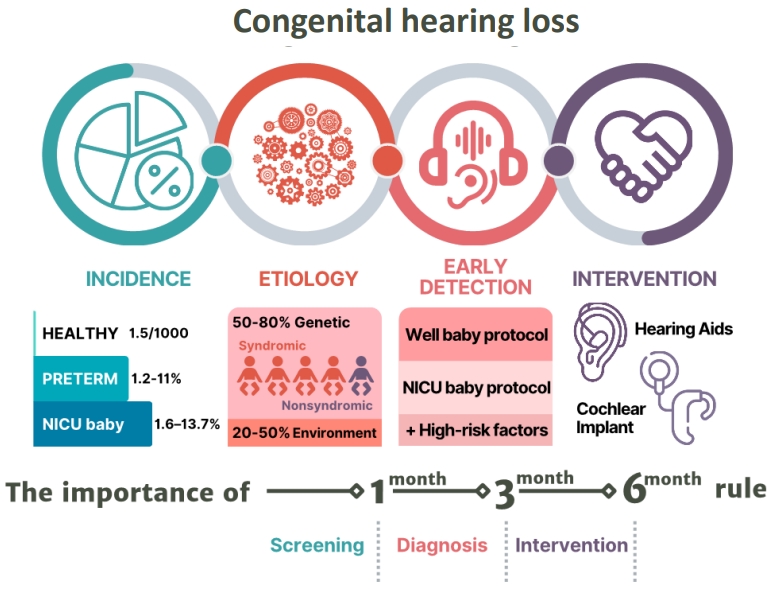
· Congenital hearing loss is common, with an approximate incidence of 1.5 per 1,000 newborns and affecting 1.2%–11% of preterm and 1.6%–13.7% of neonatal intensive care unit neonates.
· Etiologies vary, and up to 80% of cases are genetic.
· Newborn hearing screenings follow the 1-3-6 rule, and babies at high risk of hearing loss should be referred to otolaryngology for early detection and timely intervention.
- Neonatology (Perinatology)
- Neurodevelopmental outcomes of preterm infants
- In Gyu Song
- Clin Exp Pediatr. 2023;66(7):281-287. Published online December 30, 2022
-

· Among survivors, 60.9% of infants born at 22 weeks’ gestation had moderate to severe impairments, whereas 50.3% born at 23 weeks’ and 42.2% at 24 weeks’ gestation had moderate to severe impairments.
· Moderate and late preterm infants reportedly have less severe disease than very preterm infants, but they still experience adverse neurodevelopmental outcomes.
· The careful follow-up and early detection of developmental problems in these patients are required.
- Original Article
- Neonatology (Perinatology)
- A thickened formula reduces feeding-associated oxygen desaturation and bradycardia in preterm infants
- Gayoung Lee, Juyoung Lee, Ga Won Jeon, Yong Hoon Jun
- Clin Exp Pediatr. 2023;66(1):32-37. Published online December 15, 2022
-
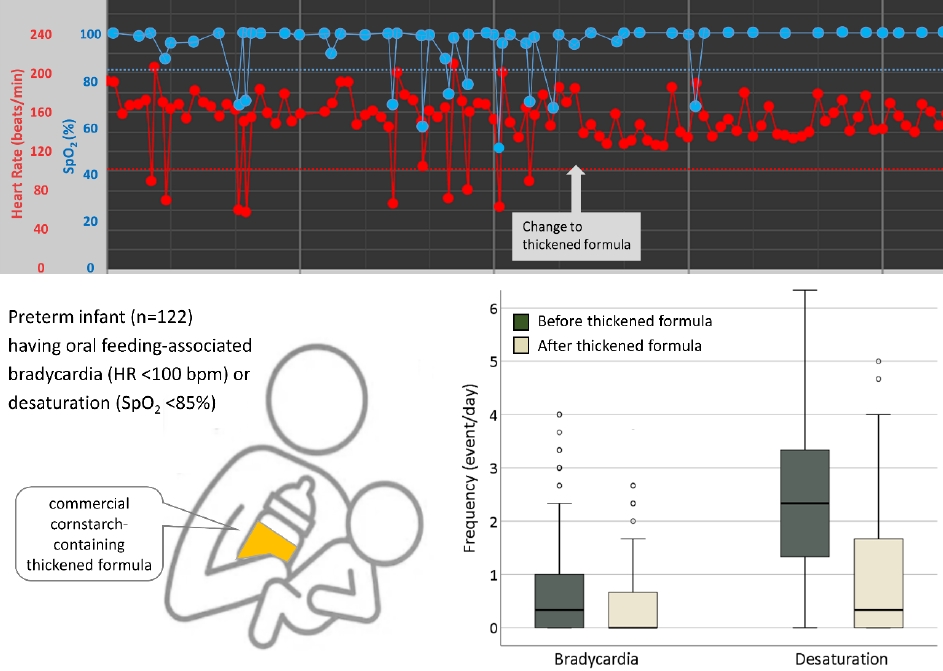
Question: Is a commercial thickened formula able to alleviate oral feeding-associated desaturation and bradycardia in preterm infants?
Finding: Thickened formula feeding significantly reduced oral feeding-associated desaturation and bradycardia in preterm infants.
Meaning: Thickened formula feeding stabilizes oxygen saturation and heart rate during oral feeding among preterm infants with feeding difficulties.
- Gastroenterology
- Probiotics added to maternal nutrition affect ınfantile colic symptoms and fecal microbiota profile: a single-blind randomized controlled study
- Aysu Yıldız Karaahmet, Gülümser Dolgun, Metehan Özen
- Clin Exp Pediatr. 2022;65(11):547-554. Published online September 23, 2022
-

Question: Do probiotics added to maternal nutrition affect infantile colic symptoms and intestinal microbiota?
Finding: Infants whose mothers ingested probiotics demonstrated decreased crying frequency and intensity and significantly increased bacterial diversity in the stools. The bacterial variety was substantially affected by the added probiotic product.
Meaning: The addition of probiotics to maternal nutrition in early infancy could play an important role in preventing infantile colic.
- Review Article
- Nephrology (Genitourinary)
- Neonatal hypertension: concerns within and beyond the neonatal intensive care unit
- Kathleen Altemose, Janis M. Dionne
- Clin Exp Pediatr. 2022;65(8):367-376. Published online May 30, 2022
-
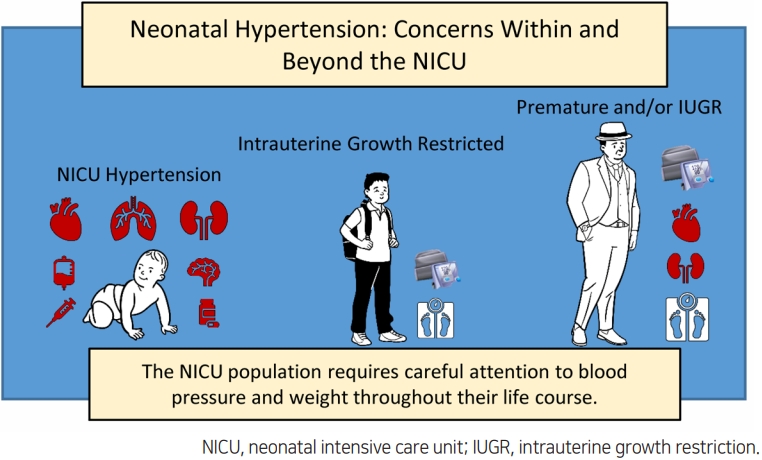
Some neonates, especially those who are premature, may experience hypertension while in the neonatal intensive care unit (NICU). The most common causes are prematurity-related and the hypertension usually resolves over the first 1–2 years of life. Unfortunately, the increasing population of NICU graduates is at risk for later cardiovascular and kidney disease in childhood and adulthood. This population requires careful attention to blood pressure and weight throughout their life course.
- Original Article
- Other
- Plastic bottle feeding produces changes in biochemical parameters in human infants – A pilot study
- Mahendra K. Pant, Abul. H. Ahmad, Manisha Naithani, Jayanti Pant
- Clin Exp Pediatr. 2022;65(9):459-465. Published online May 19, 2022
-

Question: Plastic feeding bottles are used commonly to feed infants who cannot be breastfeed. Does plastic bottle feeding produce biochemical changes in infants?
Finding: The plastic bottles leach out endocrine disruptors and affects bodily functions in terms of biochemical alterations like increased blood urea, raised creatine-kinase–MB levels, and altered lipid profile in infants exposed to bottle feeding.
Meaning: Plastic bottles feeding alters bodily functions in infants.
- Review Article
- Gastroenterology
- Clinical importance of immunonutrition in infants: a review of the recent literature
- Ji Sook Park
- Clin Exp Pediatr. 2022;65(7):337-343. Published online February 17, 2022
-

Nutrients are important in the developing immune system. Human milk supplies diverse bioactives to prevent acute infection or chronic inflammation. Immunoglobulins, lactoferrin, and glutamine in human milk decrease gastrointestinal and respiratory infection. Human milk oligosaccharides promote the growth of intestinal microbiota, the gut barrier, and antimicrobial or antiviral activity. Micronutrients act as anti-inflammatory immunonutrients, too. However, the toxicity of some nutrients from an overdose should be considered.
- Factors influencing development of the infant microbiota: from prenatal period to early infancy
- Sujin Jeong
- Clin Exp Pediatr. 2022;65(9):439-447. Published online December 23, 2021
-

∙ Microbial colonization primarily occurs after birth but there may be some colonization in utero, although this remains highly controversial.
∙ Maternal factors during pregnancy affect the infant microbiota: diet, weight, gestational weight gain, and antibiotic usage.
∙ Microbes are passed from mother-to-infant during and after birth. Delivery mode, breastfeeding, early life antibiotic, and proton pump inhibitor treatment have the largest effects on microbial composition in early life.
∙ The early life gut microbiome plays an important role in the development of the immune system and metabolism.
- Neonatology (Perinatology)
- Breastfeeding and vitamin D
- Ju Sun Heo, Young Min Ahn, Ai-Rhan Ellen Kim, Son Moon Shin; for the Korean Society of Breastfeeding Medicine
- Clin Exp Pediatr. 2022;65(9):418-429. Published online December 14, 2021
-
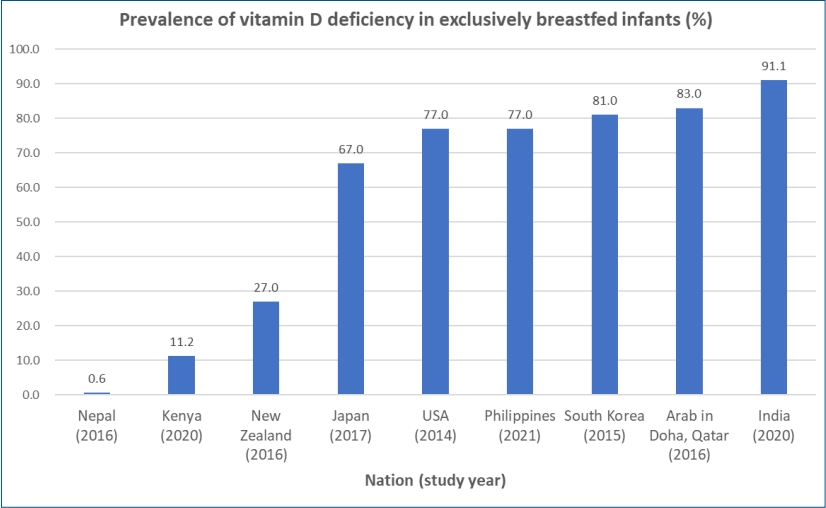
∙ Exclusively breastfed infants are at risk of developing vitamin D deficiency associated with hypocalcemia, rickets, and various health outcomes.
∙ The prevalence of vitamin D deficiency in breastfed infants differs vastly between studies and nations at 0.6%–91.1%.
∙ The vitamin D content of breast milk does not meet the requirements of exclusively breastfed infants.
∙ Most international guidelines recommend that breastfed infants be supplemented with 400 IU/day of vitamin D during the first year of life.
∙ Vitamin D intake (milk+supplements) of 800 IU/day can be considered in preterm infants along with biochemical monitoring.
- Original Article
- Other
- Risk factors and screening timing for developmental dysplasia of the hip in preterm infants
- Ga Won Jeon, Hye Jung Choo, Yong Uk Kwon
- Clin Exp Pediatr. 2022;65(5):262-268. Published online November 5, 2021
-

Question: When is the best screening timing and what is the risk factor for developmental dysplasia of the hip (DDH) in preterm infants?
Finding: Ultrasonography performed earlier than 38 weeks of postmenstrual age caused unnecessary subsequent ultrasonography. DDH did not occur predominantly on the left side or in breech infants.
Meaning: The screening timing, etiology, and risk factors for DDH in preterm infants are somewhat different from those in term infants.
- Review Article
- Neonatology (Perinatology)
- Pathophysiology, classification, and complications of common asymptomatic thrombocytosis in newborn infants
- Ga Won Jeon
- Clin Exp Pediatr. 2022;65(4):182-187. Published online October 18, 2021
-
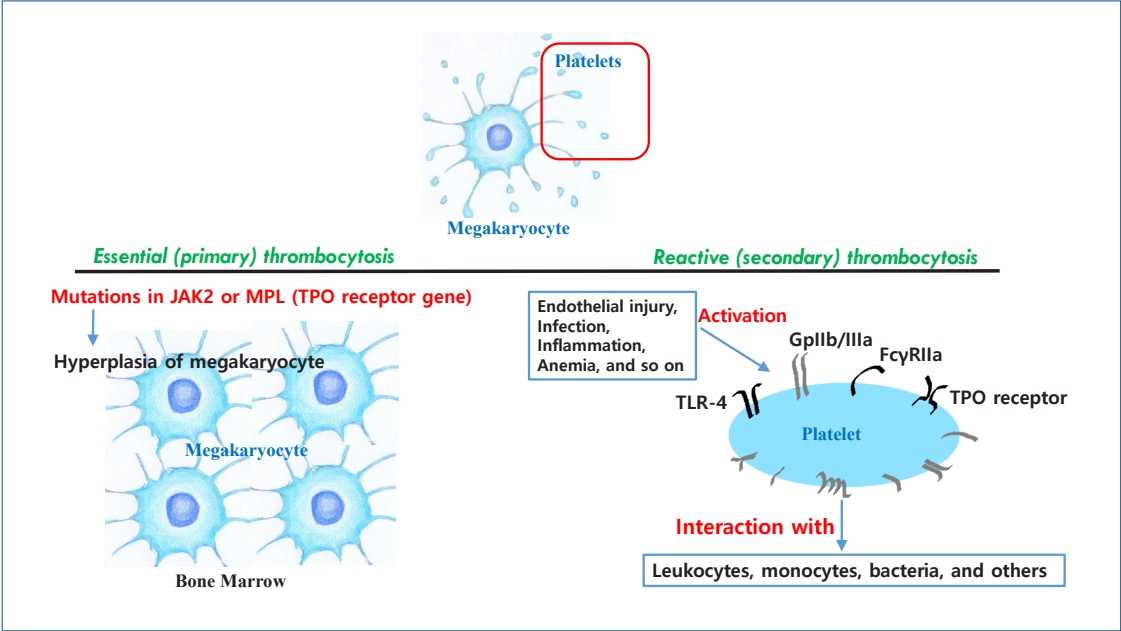
· Thrombocytosis, common in newborns and infants (<2 years) (3%–13%), is caused by elevated thrombopoietin (TPO) concentrations.
· Serum TPO levels are significantly higher immediately to 1 month postnatal and decrease with age.
· Platelet counts are positively correlated with gestational age at birth and postnatal age.
· Thrombocytosis is more common in preterm than in term infants.
· Thrombocytosis in newborns is reactive and resolves spontaneously without complications.
- Original Article
- Neonatology (Perinatology)
- Comparison of minimally invasive surfactant therapy with intubation surfactant administration and extubation for treating preterm infants with respiratory distress syndrome: a randomized clinical trial
- Mohammad Kazem Sabzehei, Behnaz Basiri, Maryam Shokouhi, Sajad Ghahremani, Ali Moradi
- Clin Exp Pediatr. 2022;65(4):188-193. Published online July 28, 2021
-

Question: Are the short-term outcomes of minimally invasive surfactant therapy (MIST) relatively superior to those of INtubation, SURfactant administration, and Extubation (INSURE) in preterm infants with respiratory distress syndrome (RDS)?
Finding: MIST could be an appropriate substitution for INSURE in preterm infants with RDS since it reduced hospitalization time and number of side effects.
Meaning: MIST is recommended for surfactant administration for its proven advantages over the INSURE technique.
- Review Article
- Neonatology (Perinatology)
- Growth patterns of preterm infants in Korea
- Joohee Lim, So Jin Yoon, Soon Min Lee
- Clin Exp Pediatr. 2022;65(1):1-9. Published online July 8, 2021
-
∙ The growth of preterm infants is a main focus of neonatology.
∙ Preterm infants in Korea, especially those with a very low birth weight, achieve retarded growth.
∙ Careful growth monitoring and early intervention will contribute to better development outcomes and quality of life for preterm infants and improve public health.
- Infection
- Recommendation for use of diphtheria and tetanus toxoids and acellular pertussis, inactivated poliovirus, Haemophilus influenzae type b conjugate, and hepatitis B vaccine in infants
- Hye-Kyung Cho, Su Eun Park, Yae-Jean Kim, Dae Sun Jo, Yun-Kyung Kim, Byung-Wook Eun, Taek-Jin Lee, Jina Lee, Hyunju Lee, Ki Hwan Kim, Eun Young Cho, Jong Gyun Ahn, Eun Hwa Choi; The Committee on Infectious Diseases of the Korean Pediatric Society
- Clin Exp Pediatr. 2021;64(12):602-607. Published online June 8, 2021
-
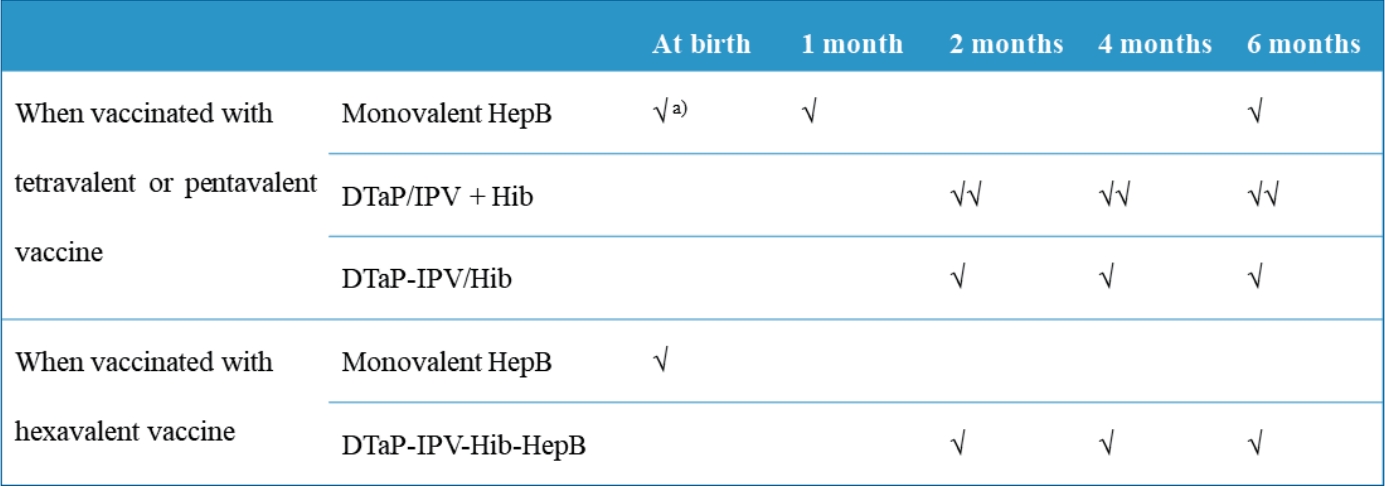
∙ Diphtheria and tetanus toxoids and acellular pertussis-inactivated poliovirus-Haemophilus influenzae type b-hepatitis B (DTaP-IPV-Hib-HepB) was licensed in Korea in April 2020.
∙ DTaP-IPV-Hib-HepB is indicated as a 3-dose primary series for infants aged 2, 4, and 6 months who received the standalone HepB vaccine at birth.
∙ Infants born to HepB surface antigen-positive mothers are currently recommended to be immunized with HepB immunoglobulin at birth and then monovalent HepB vaccine at 0, 1, and 6 months.
- Original Article
- General Pediatrics
- Efficacy of probiotics for managing infantile colic due to their anti-inflammatory properties: a meta-analysis and systematic review
- Reza Shirazinia, Ali Akbar Golabchifar, Mohammad Reza Fazeli
- Clin Exp Pediatr. 2021;64(12):642-651. Published online April 12, 2021
-
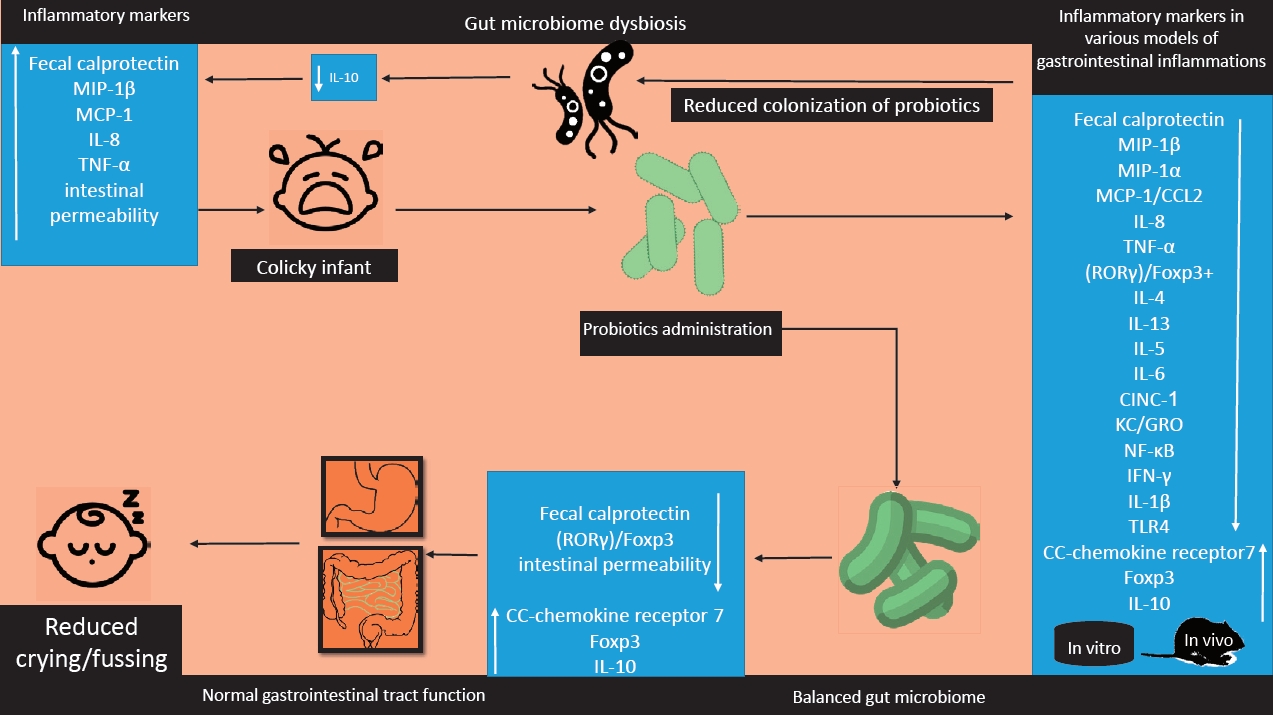
Question: Do probiotics reduce colic symptoms?
Finding: Probiotics reduced colic symptoms in colicky infants probably due to the anti-inflammatory properties.
Meaning: Probiotics may be an effective and less noxious way to manage infantile colic.
-

-
-
6.02024CiteScore98th percentilePowered by
-
Impact Factor3.6
-
- TOPICS
- ARTICLE CATEGORY
- Editorial Office
-
Korean Pediatric Society
#1606 Seocho World Officetel, 19 Seoun-ro, Seocho-ku, Seoul 06732, Korea
Tel: +82-2-3473-7306 Fax: +82-2-3473-7307 E-mail: office@e-cep.org
Clinical and Experimental Pediatrics is an open access journal. All articles are distributed under the terms of the Creative Commons Attribution NonCommercial License (http://creativecommons.org/licenses/by-nc/4.0/)
Copyright © 2025 by Korean Pediatric Society.