Neonatology (Perinatology)
- Page Path
-
- HOME
- TOPICS
- Neonatology (Perinatology)
- Topics
-
- Adolescence Medicine (3)
- Allergy (53)
- Cardiology (76)
- Critical Care Medicine (8)
- Developmental and Behavioral Medicine (19)
- Emergency Medicine (5)
- Endocrinology (53)
- Gastroenterology (57)
- General Pediatrics (38)
- Genetics and Metabolism (22)
- Hematology (12)
- Immunology (12)
- Infection (66)
- Neonatology (Perinatology) (108)
- Nephrology (Genitourinary) (49)
- Neurology (88)
- Nutrition (26)
- Oncology (15)
- Neurobehavior (12)
- Pulmonology (26)
- Rheumatology (2)
- Other (30)
- Letter to the Editor
- Neonatology (Perinatology)
- Pentraxin 3 as a marker of early-onset neonatal sepsis
- Safaa ELMeneza, Iman El-Bagoury, Hind Rayes, Amira Hassan
- Clin Exp Pediatr. 2024;67(6):312-314. Published online May 23, 2024
-

- Original Article
- Neonatology (Perinatology)
- Effect of vitamin E supplementation on bilirubin levels in infants with hyperbilirubinemia: a double-blind randomized clinical trial
- Mojtaba Cheraghi, Maziar Nikouei, Majid Mansouri, Siros Hemmatpour, Yousef Moradi
- Clin Exp Pediatr. 2024;67(5):249-256. Published online March 26, 2024
-
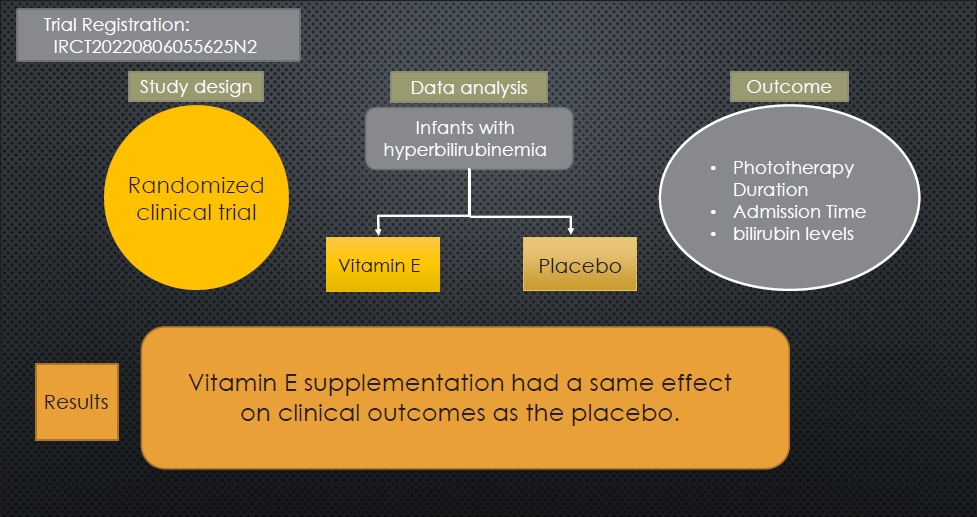
Question: Is vitamin E a viable therapeutic option for managing neonatal hyperbilirubinemia?
Finding: This randomized clinical trial examined the effects of oral vitamin E supplementation on bilirubin reduction (primary outcome), phototherapy duration, and length of hospital stay (secondary outcome) in 138 infants.
Meaning: Infants administered vitamin E versus placebo demonstrated similar reductions in bilirubin levels and length of hospital stay.
- Editorial
- Neonatology (Perinatology)
- Exploring the role of laryngeal masks in neonatal resuscitation
- Euiseok Jung
- Clin Exp Pediatr. 2024;67(5):247-248. Published online December 28, 2023
-
· Laryngeal masks (LMs) offer stable airway access and skill retention advantages, making them promising alternatives to positive-pressure ventilation in neonatal care.
· The ease of teaching LM insertion techniques to less experienced providers addresses the need for swift intervention and skill retention.
· Careful consideration of the benefits and challenges of LMs is essential in determining their effective integration into enhanced neonatal resuscitation protocols.
- Review Article
- Neonatology (Perinatology)
- Updates in neonatal resuscitation: routine use of laryngeal masks as an alternative to face masks
- Eun Song Song, Ga Won Jeon
- Clin Exp Pediatr. 2024;67(5):240-246. Published online July 11, 2023
-

In neonatal resuscitation:
· Laryngeal masks are recommended when endotracheal intubation or positive-pressure ventilation fails.
· Laryngeal masks are useful even during chest compressions.
· Laryngeal masks aid neonates >34 weeks’ gestation and/or with a birth weight >2 kg.
· Main usage barriers include limited experience (81%), preference for endotracheal tubes (57%), and lack of awareness (56%).
· Second-generation laryngeal masks have a built-in esophageal drainage tube that prevents regurgitation into the glottis, and an orogastric tube can be inserted within the esophageal drainage tube to protect against gastric inflation.
- Influence of infant microbiome on health and development
- Noelle Younge
- Clin Exp Pediatr. 2024;67(5):224-231. Published online August 21, 2023
-

· The infant gut microbiome is highly dynamic and individualized.
· Microbes are vertically transmitted from mother to infant during delivery and throughout infancy.
· Delivery mode, gestational age, diet, and antibiotic use influence infant microbiome composition and function.
· In animal studies, the microbiome played critical roles in the structural and functional development of the infant gastrointestinal and immune systems.
· Microbiome-targeted therapies have great potential to reduce infant morbidity and mortality.
- Letter to the Editor
- Neonatology (Perinatology)
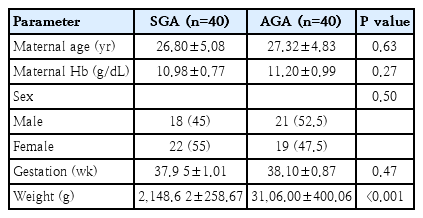
- Assessment of iron status and red cell parameters in healthy term small for gestational age neonates at birth
- Arif Hossain, Shorna Rahman, Shahana Akter, Ismat Jahan, Sanjoy Kumer Dey, Abdul Mannan, Mohammod Shahidullah
- Clin Exp Pediatr. 2024;67(4):221-223. Published online March 19, 2024
-
- Review Article
- Neonatology (Perinatology)
- Neonatal family-centered care: evidence and practice models
- Juyoung Lee
- Clin Exp Pediatr. 2024;67(4):171-177. Published online June 14, 2023
-
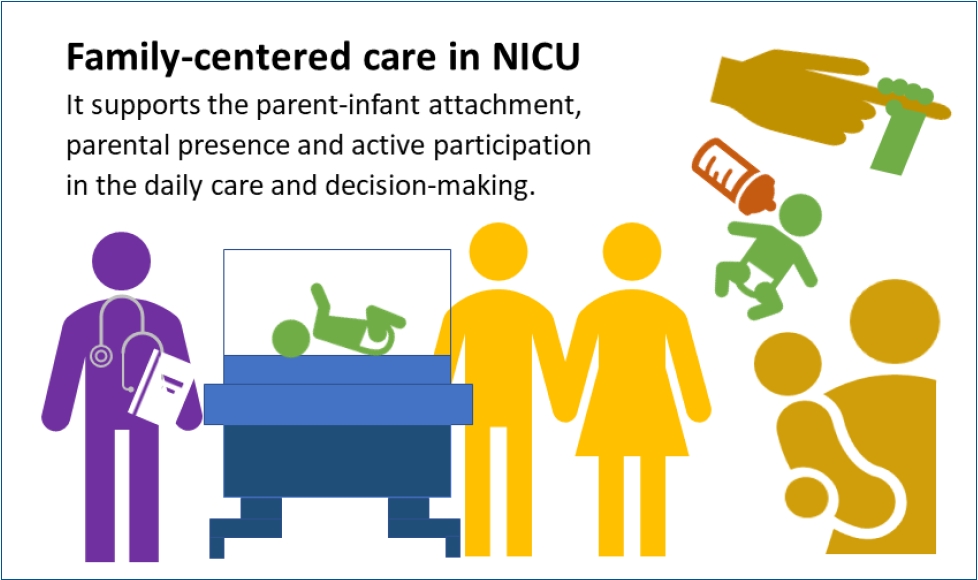
· Concrete evidence exists of early parent-infant attachment supported by family-centered care (FCC) in the neonatal intensive care unit.
· FCC involves the parents’ presence and participation in the infant’s care and decision-making.
· A private and comfortable space should be provided. A single-family room is ideal; however, a quiet space with a recliner can be a good alternative.
· Care culture changes and staff training are required.
- Original Article
- Neonatology (Perinatology)
- Oral administration of bone marrow-derived mesenchymal stem cells attenuates intestinal injury in necrotizing enterocolitis
- Yeong Seok Lee, Yong Hoon Jun, Juyoung Lee
- Clin Exp Pediatr. 2024;67(3):152-160. Published online February 19, 2024
-
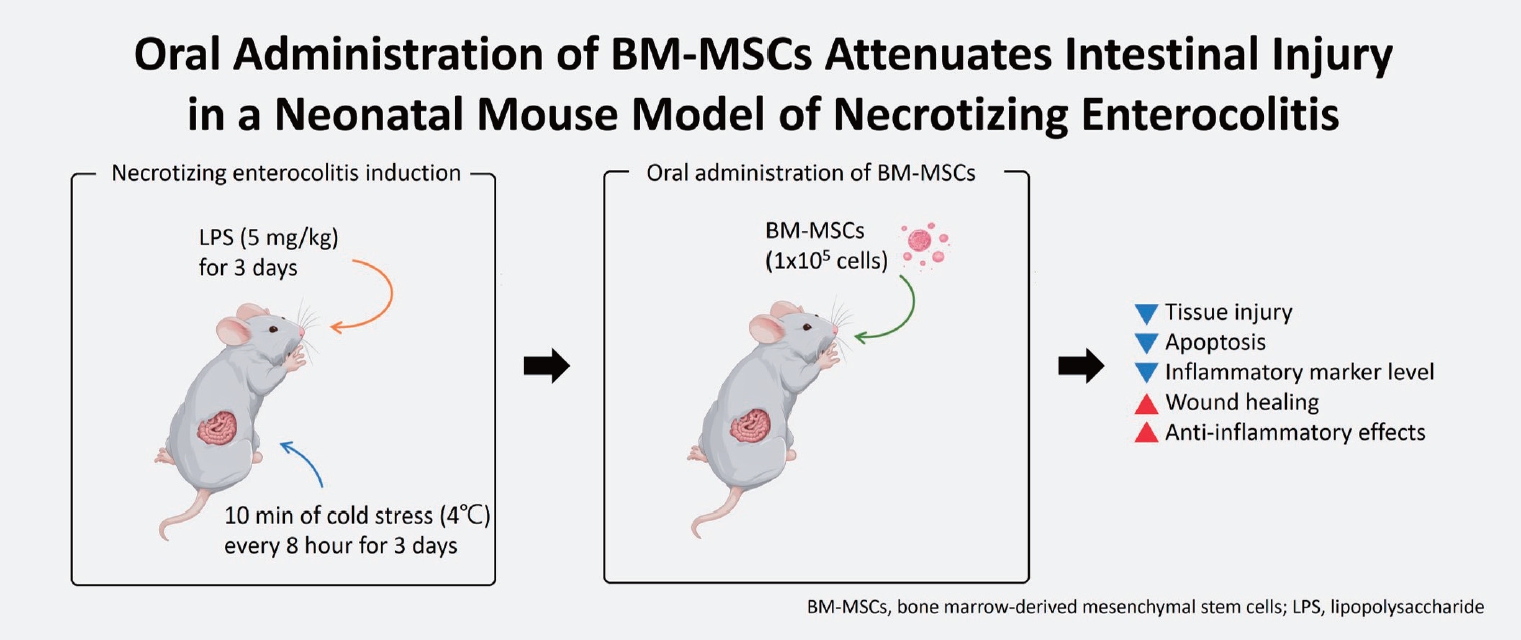
Question: What is the optimal dose of bone marrow-derived mesenchymal stem cells (BM-MSCs) for treating necrotizing enterocolitis (NEC), and is orally administered BM-MSC effective?
Findings: High (1×106 cells) or multiple BM-MSC doses showed similar effects as low (1×105 cells) doses of intraperitoneally administered BM-MSCs. Furthermore, orally administered BM-MSCs were as effective as intraperitoneally administered BM-MSCs.
Meaning: Orally administered low-dose BM-MSCs are a potential treatment for NEC.
- Editorial
- Neonatology (Perinatology)
- Impacts of maternal COVID-19 during pregnancy on neonatal health and epidemiology
- Jae Woo Lim
- Clin Exp Pediatr. 2024;67(3):149-151. Published online December 28, 2023
-

Newborns born to mothers infected with coronavirus disease 2019 (COVID-19) should be closely monitored for respiratory disorders, such as transient tachypnea of the newborn, regardless of their COVID-19 test results. Further research is required of the development of infants born to mothers with COVID-19. The trends in Korea's birth rate and infant mortality rates have not been significantly affected by COVID-19.
- Original Article
- Neonatology (Perinatology)
- Prevalence of anxiety, depression, and stress among parents of neonates admitted to neonatal intensive care unit: a systematic review and meta-analysis
- Asha P. Shetty, Kurvatteppa Halemani, Alwin Issac, Latha Thimmappa, Sanjay Dhiraaj, Radha K, Prabhaker Mishra, Vijai Datta Upadhyaya
- Clin Exp Pediatr. 2024;67(2):104-115. Published online November 14, 2023
-
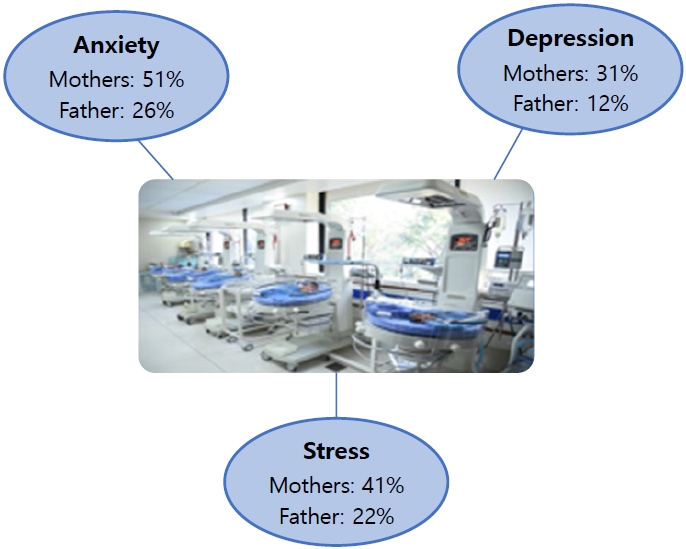
Question: What emotions do parents experience when their newborns are admitted to the neonatal intensive care unit (NICU)?
Finding: Mothers experienced more anxiety (51%), depression (31%), and stress (41%) symptoms than fathers (26%, 12%, and 22%, respectively).
Meaning: Parents often experience anxiety, stress, and depression following NICU admission. Healthcare workers are responsible for providing regular parental counseling.
- Letter to the Editor
- Neonatology (Perinatology)
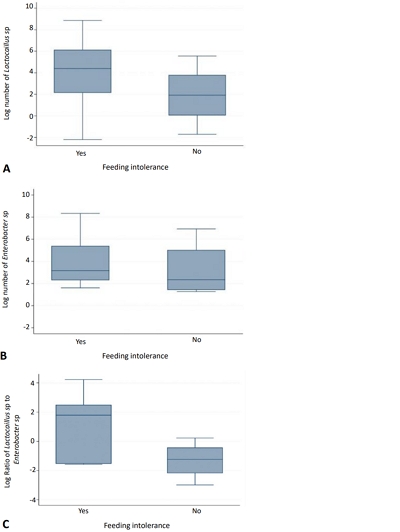
- Association between feeding intolerance and intestinal dysbiosis in very premature infants
- Putri Maharani Tristanita Marsubrin, Agus Firmansyah, Rinawati Rohsiswatmo, Zakiudin Munasir, Saptawati Bardosono, Safarina G. Malik, Yuditiya Purwosunu, Ina S. Timan, Tetty Yuniati, Maya Yulindhini
- Clin Exp Pediatr. 2023;66(11):501-503. Published online October 24, 2023
-
- Original Article
- Neonatology (Perinatology)
- Association between maternal coronavirus disease 2019 and transient tachypnea of the newborn: a single-center study
- Sung Hee Lee, Ju Hyun Jin, Jong Ha Yoo, Shin Won Yoon
- Clin Exp Pediatr. 2023;66(11):493-500. Published online October 24, 2023
-
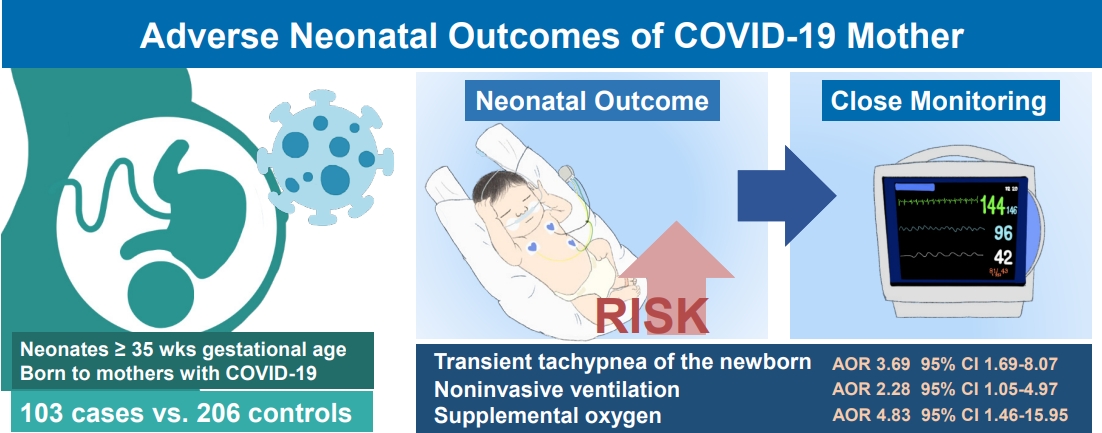
Question: What are the adverse clinical outcomes of neonates of coronavirus disease 2019 (COVID-19)–infected mothers?
Finding: Infants of mothers with COVID-19 were at significantly increased risk of transient tachypnea of the newborn (TTN), use of noninvasive ventilation, and need for supplemental oxygen (P<0.05).
Meaning: Neonates of mothers with COVID-19 are at risk of TTN and require respiratory support. Close monitoring is essential to ensuring timely intervention if required.
- Review Article
- Neonatology (Perinatology)
- Treatment of congenital cytomegalovirus infection
- Gyu Hong Shim
- Clin Exp Pediatr. 2023;66(9):384-394. Published online December 28, 2022
-
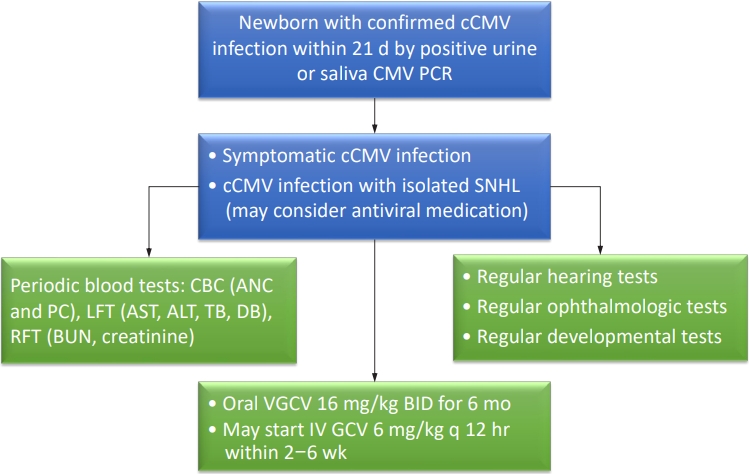
· Congenital cytomegalovirus (CMV) infection is among the most common causes of nongenetic sensorineural hearing loss.
· Congenital CMV is initially treated with intravenous ganciclovir for 2–6 weeks and switched to oral valganciclovir, or with oral valganciclovir for the entire 6-month period.
· Infants with congenital CMV require periodic monitoring of absolute neutrophil count, platelet count, and blood urea nitrogen, creatinine, liver function tests, audiological, ophthalmological, and developmental tests during antiviral medication.
- Neurodevelopmental outcomes of preterm infants
- In Gyu Song
- Clin Exp Pediatr. 2023;66(7):281-287. Published online December 30, 2022
-

· Among survivors, 60.9% of infants born at 22 weeks’ gestation had moderate to severe impairments, whereas 50.3% born at 23 weeks’ and 42.2% at 24 weeks’ gestation had moderate to severe impairments.
· Moderate and late preterm infants reportedly have less severe disease than very preterm infants, but they still experience adverse neurodevelopmental outcomes.
· The careful follow-up and early detection of developmental problems in these patients are required.
- Original Article
- Neonatology (Perinatology)
- Efficacy of body position on gastric residual in preterm infant: a systematic review and meta-analysis
- Kurvatteppa Halemani, Alwin Issac, Sanjay Dhiraaj, Prabhaker Mishra
- Clin Exp Pediatr. 2023;66(6):262-270. Published online November 30, 2022
-
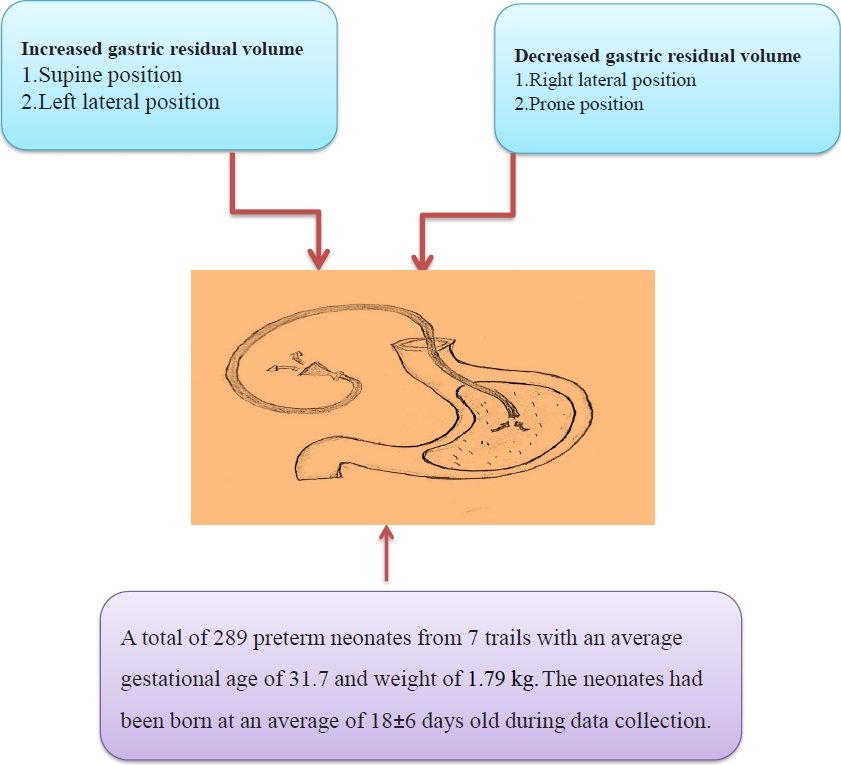
Breastfeeding and it's tolerance are the positive indicators for preterm babies. Placing the preterm infant in the right lateral or prone position after feed had lesser gastric residual volume compared to placing them in left lateral or supine positions. The post-feed position is a vital element in enhancing feeding tolerance, mechanical functions of the gastrointestinal tract and the overall development of preterm infants.
- A thickened formula reduces feeding-associated oxygen desaturation and bradycardia in preterm infants
- Gayoung Lee, Juyoung Lee, Ga Won Jeon, Yong Hoon Jun
- Clin Exp Pediatr. 2023;66(1):32-37. Published online December 15, 2022
-
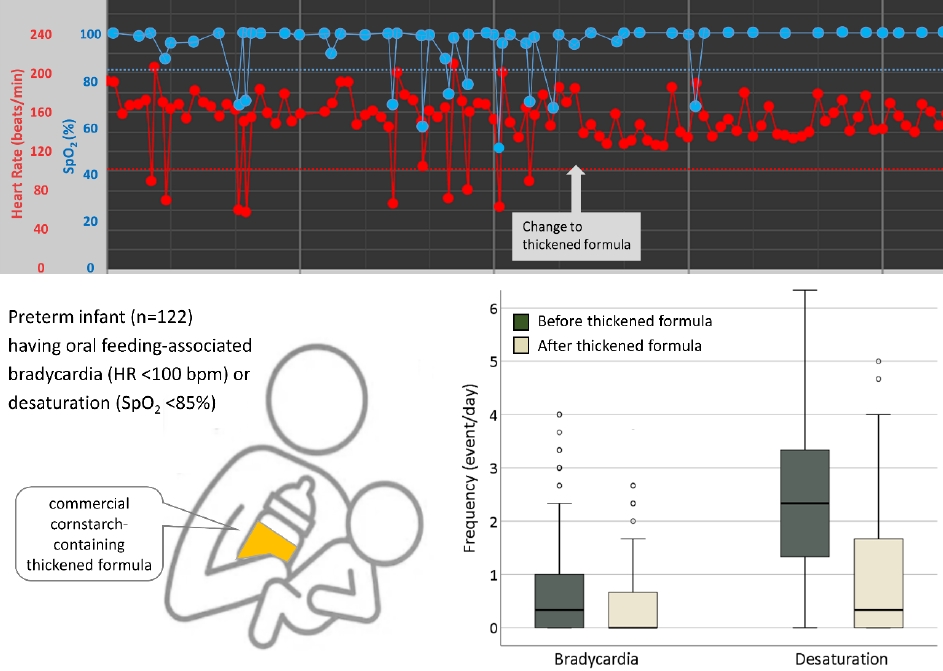
Question: Is a commercial thickened formula able to alleviate oral feeding-associated desaturation and bradycardia in preterm infants?
Finding: Thickened formula feeding significantly reduced oral feeding-associated desaturation and bradycardia in preterm infants.
Meaning: Thickened formula feeding stabilizes oxygen saturation and heart rate during oral feeding among preterm infants with feeding difficulties.
- Editorial
- Neonatology (Perinatology)
- Does cord blood cortisol have a mediating effect on maternal prepregnancy body mass index and birth weight?
- Gyu Hong Shim
- Clin Exp Pediatr. 2023;66(1):24-25. Published online November 30, 2022
-

· A high prepregnancy body mass index (pre-BMI) is associated with large for gestational age (LGA) and macrosomia, whereas a low pre-BMI is associated with small for gestational age (SGA) and low birth weight (LBW).
· The identification of the role of the hypothalamus-pituitary-adrenal axis in the effect of pre-BMI and maternal gestational weight gain on birth weight could reduce the frequency of LGA, macrosomia, SGA, or LBW through maternal diet optimization.
- Review Article
- Neonatology (Perinatology)
- Neonatal seizures: stepping outside the comfort zone
- Menna Hashish, Mohamed Reda Bassiouny
- Clin Exp Pediatr. 2022;65(11):521-528. Published online April 4, 2022
-

· Use conventional and amplitude-integrated electroencephalography to confirm clinical seizures and screen high-risk newborns.
· Select an explicit clear elective event to be treated with less toxic and more effective antiepileptics.
- Original Article
- Neonatology (Perinatology)
- Mediation effect of cord blood cortisol levels between maternal prepregnancy body mass index and birth weight: a hospital-based cross-sectional study
- Nisanth Selvam, Jayashree K, Prasanna Mithra
- Clin Exp Pediatr. 2022;65(10):500-506. Published online July 29, 2022
-

Question: What is the association between cord blood cortisol and maternal weight, birth weight, and cord blood lipid profile?
Finding: Cord blood cortisol levels did not influence the relationship between maternal weight changes or birth weight. Maternal weight changes, birth weight, and cortisol levels altered the cord blood lipid profile.
Meaning: Our findings may aid United Nations Sustainable Development Goal 3 (Good Health and Well-Being) achievement by 2030.
- Review Article
- Neonatology (Perinatology)
- Breastfeeding and vitamin D
- Ju Sun Heo, Young Min Ahn, Ai-Rhan Ellen Kim, Son Moon Shin; for the Korean Society of Breastfeeding Medicine
- Clin Exp Pediatr. 2022;65(9):418-429. Published online December 14, 2021
-
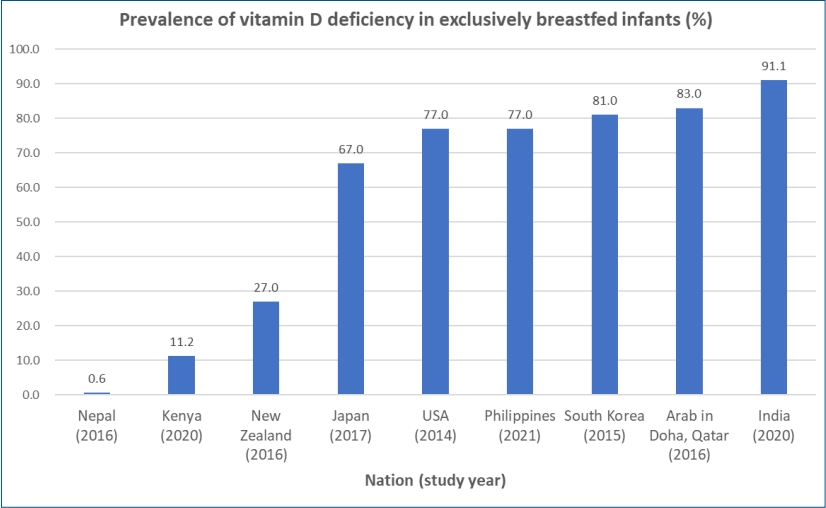
∙ Exclusively breastfed infants are at risk of developing vitamin D deficiency associated with hypocalcemia, rickets, and various health outcomes.
∙ The prevalence of vitamin D deficiency in breastfed infants differs vastly between studies and nations at 0.6%–91.1%.
∙ The vitamin D content of breast milk does not meet the requirements of exclusively breastfed infants.
∙ Most international guidelines recommend that breastfed infants be supplemented with 400 IU/day of vitamin D during the first year of life.
∙ Vitamin D intake (milk+supplements) of 800 IU/day can be considered in preterm infants along with biochemical monitoring.
- Editorial
- Neonatology (Perinatology)
- Factors to consider before implementing telemedicine protocols to manage neonatal jaundice
- Heui Seung Jo
- Clin Exp Pediatr. 2022;65(8):403-404. Published online April 12, 2022
-
In the rapidly changing environmental situation during the coronavirus disease 2019 outbreak, neonatal centers have developed telemedicine systems with extended coverage for neonatal monitoring and high-risk follow-up programs including neonatal hyperbilirubinemia. At this point, electronic health technology and noncontact medical system increase the effectiveness of rather than replacing the face-to-face visit and the opinions of experienced neonatologists.
- Original Article
- Neonatology (Perinatology)
- Neonatal sepsis-causing bacterial pathogens and outcome of trends of their antimicrobial susceptibility a 20-year period at a neonatal intensive care unit
- Woo Sun Song, Hye Won Park, Moon Youn Oh, Jae Young Jo, Chae Young Kim, Jung Ju Lee, Euiseok Jung, Byong Sop Lee, Ki-Soo Kim, Ellen Ai-Rhan Kim
- Clin Exp Pediatr. 2022;65(7):350-357. Published online December 9, 2021
-
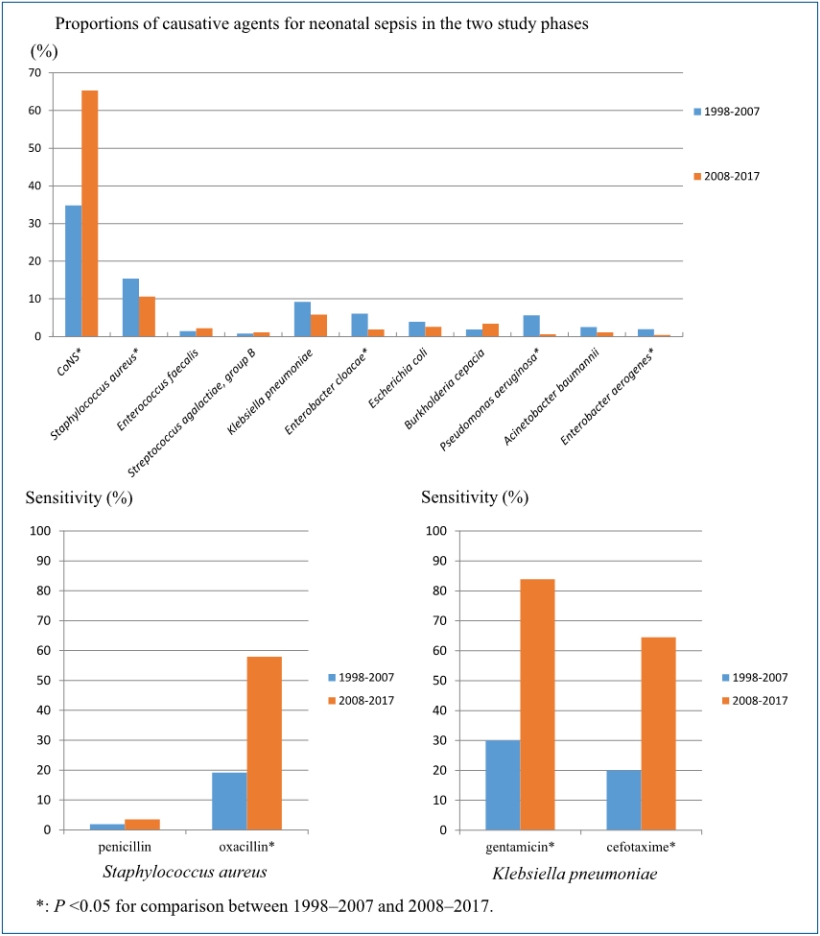
Question: What is prevalence of bacterial pathogens causing sepsis and their antimicrobial susceptibility over 20 years?
Finding: Coagulase-negative remains most common causative organism. The most common gram-negative organism was Klebsiella pneumonia. The susceptibility of staphylococcus aureus and K. pneumonia showed increased susceptability to oxacillin, cefotaxime and amikacin, gentamicin, respectively.
Meaning: Answers to the question asked is important in choosing antimicrobials and to monitor emergence of multidrug-resistant organisms.
- Editorial
- Neonatology (Perinatology)
- Ideal timing for aggressive screening to detect developmental dysplasia of the hip in term and preterm infants
- Won-Ho Hahn
- Clin Exp Pediatr. 2022;65(7):346-347. Published online March 14, 2022
-

The risk factors and pathogenesis of developmental dysplasia of the hip (DDH) are unclear. Moreover, no universal screening method can entirely eliminate the risk of DDH. However, its incidence is significant and its early detection is critical for improving patient prognosis. Although the ideal evaluation time and risk factors, especially for premature infants, are unclear, the necessity for DDH screening programs for term and preterm infants is emerging.
- Letter to the Editor
- Neonatology (Perinatology)
- Telemedicine as progressive treatment approach for neonatal jaundice due to the coronavirus disease 2019 pandemic
- Sukanya Sudhir Joshi, Bithiah Roy Benroy, Isabell Nelson Lawrence, Thanuja Jayasri Suresh
- Clin Exp Pediatr. 2022;65(5):269-271. Published online February 7, 2022
-
Question: How can the management of neonatal jaundice (NJ) be enhanced through telemedicine?
Finding: Teleconsultations, drive-through testing, and the use of an application to assess neonatal jaundice at home are being successfully used, but they must be further researched before being implemented on a larger scale.
Meaning: Recent technology allows for the treatment of NJ at home with an application that helps reduce hospital burden.
- Original Article
- Neonatology (Perinatology)
- Comparison of minimally invasive surfactant therapy with intubation surfactant administration and extubation for treating preterm infants with respiratory distress syndrome: a randomized clinical trial
- Mohammad Kazem Sabzehei, Behnaz Basiri, Maryam Shokouhi, Sajad Ghahremani, Ali Moradi
- Clin Exp Pediatr. 2022;65(4):188-193. Published online July 28, 2021
-

Question: Are the short-term outcomes of minimally invasive surfactant therapy (MIST) relatively superior to those of INtubation, SURfactant administration, and Extubation (INSURE) in preterm infants with respiratory distress syndrome (RDS)?
Finding: MIST could be an appropriate substitution for INSURE in preterm infants with RDS since it reduced hospitalization time and number of side effects.
Meaning: MIST is recommended for surfactant administration for its proven advantages over the INSURE technique.
- Review Article
- Neonatology (Perinatology)
- Pathophysiology, classification, and complications of common asymptomatic thrombocytosis in newborn infants
- Ga Won Jeon
- Clin Exp Pediatr. 2022;65(4):182-187. Published online October 18, 2021
-
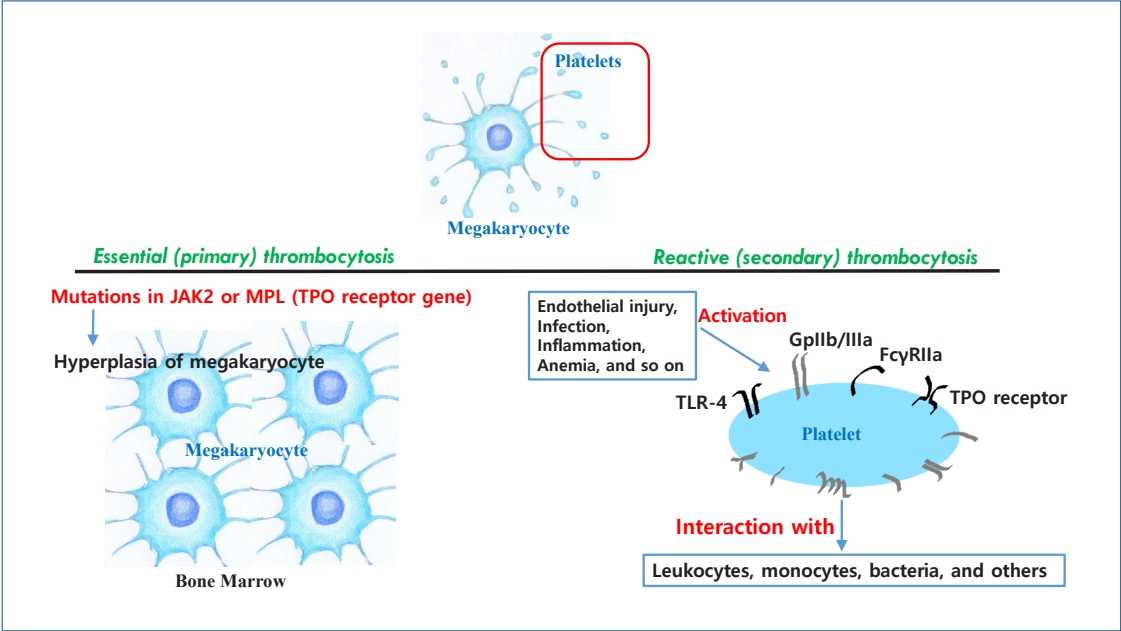
· Thrombocytosis, common in newborns and infants (<2 years) (3%–13%), is caused by elevated thrombopoietin (TPO) concentrations.
· Serum TPO levels are significantly higher immediately to 1 month postnatal and decrease with age.
· Platelet counts are positively correlated with gestational age at birth and postnatal age.
· Thrombocytosis is more common in preterm than in term infants.
· Thrombocytosis in newborns is reactive and resolves spontaneously without complications.
- Original Article
- Neonatology (Perinatology)
- Is fetal nuchal cord associated with autism spectrum disorder? A meta-analysis
- Ensiyeh Jenabi, Maryam Ahmadi, Azam Maleki
- Clin Exp Pediatr. 2022;65(3):131-135. Published online September 24, 2021
-
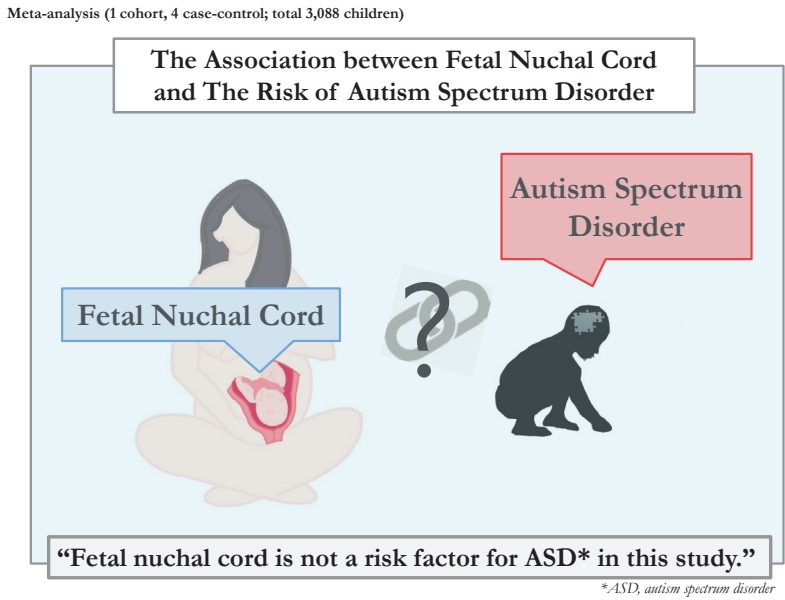
Question: Is fetal nuchal cord a risk factor for autism spectrum disorder (ASD)?
Finding: Five articles (1 cohort, 4 case-control; total 3,088 children) were included in the present meta-analysis. Fetal nuchal cord was not a risk factor for ASD (odds ratio, 1.11; 95% confidence interval, 0.66–1.57). There was homogeneity among studies that reported a risk of ASD (I2=0.0).
Meaning: Fetal nuchal cord is not a risk factor for ASD.
- Review Article
- Neonatology (Perinatology)
- Retinopathy of prematurity: a review of epidemiology and current treatment strategies
- Eun Hee Hong, Yong Un Shin, Heeyoon Cho
- Clin Exp Pediatr. 2022;65(3):115-126. Published online October 12, 2021
-
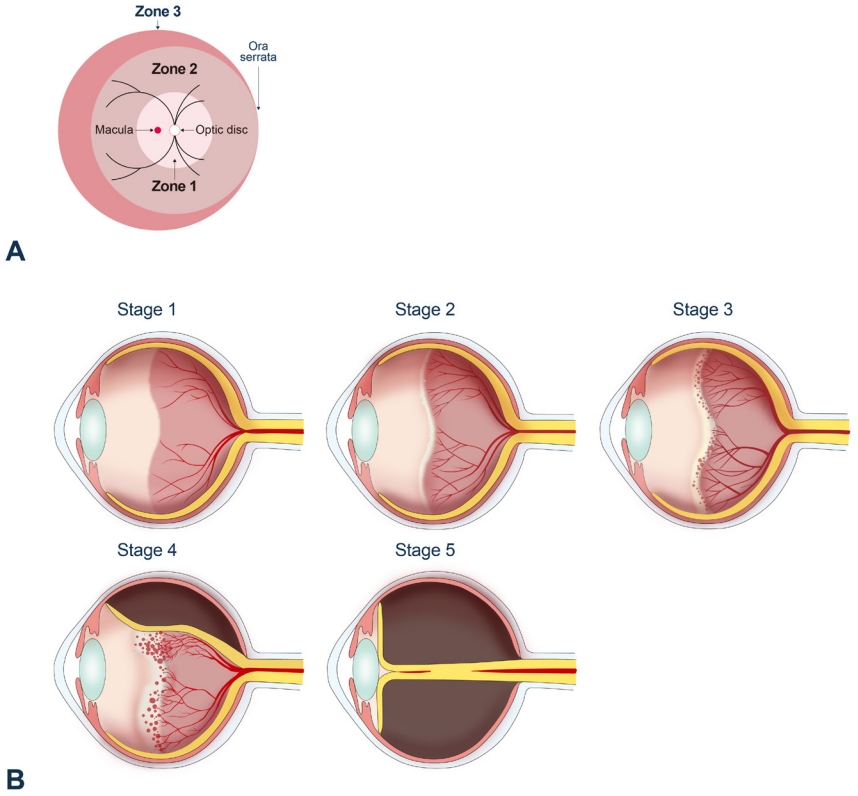
There have been global tri-phasic epidemic periods of retinopathy of prematurity (ROP). In recent years, its incidence has reportedly been 10%–40% depending on country and study population. Current treatment strategies for ROP include laser photocoagulation, surgical treatment, and anti-vascular endothelial growth factor treatment, the role of which has drawn attention in recent years.
- Growth patterns of preterm infants in Korea
- Joohee Lim, So Jin Yoon, Soon Min Lee
- Clin Exp Pediatr. 2022;65(1):1-9. Published online July 8, 2021
-
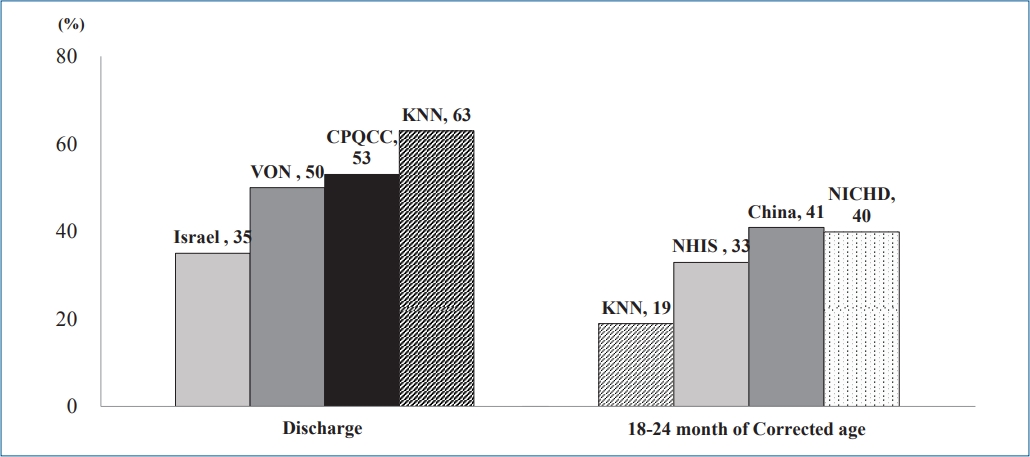
∙ The growth of preterm infants is a main focus of neonatology.
∙ Preterm infants in Korea, especially those with a very low birth weight, achieve retarded growth.
∙ Careful growth monitoring and early intervention will contribute to better development outcomes and quality of life for preterm infants and improve public health.
- Original Article
- Neonatology (Perinatology)
- Effects of carnosine and hypothermia combination therapy on hypoxic-ischemic brain injury in neonatal rats
- Jun Chul Byun, Seong Ryong Lee, Chun Soo Kim
- Clin Exp Pediatr. 2021;64(8):422-428. Published online February 24, 2021
-
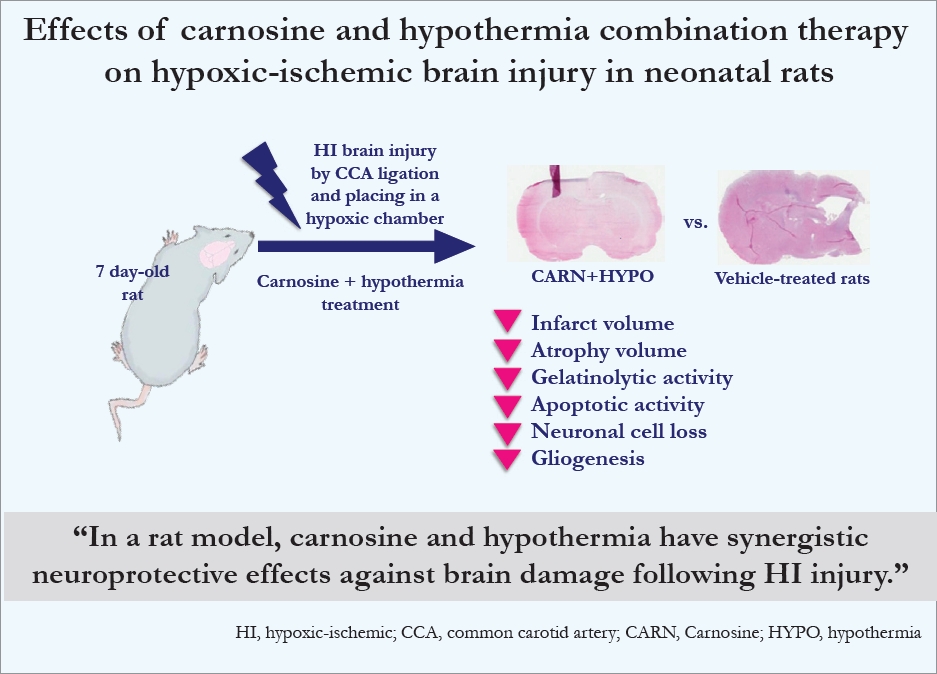
Question: How can we further improve the neuroprotective effects of hypothermia in newborns with hypoxic-ischemic (HI) brain injury?
Finding: Combination carnosine and hypothermia therapy effectively reduced brain damage in neonatal rats. The in situ zymography, terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling assay, and immunofluorescence study results showed that neuroprotective effects were achieved with combination therapy only.
Meaning: Carnosine and hypothermia have synergistic neuroprotective effects against brain damage following HI injury
-

-
-

-
-
Impact Factor3.2
-
8.02023CiteScore94nd percentilePowered by







